Osteogenesis imperfecta (brittle bone disease) is a genetic disease that makes your bones thin and brittle. People with osteogenesis imperfecta break bones easily, with little or no force causing the break. It can also cause a curved spine, muscle weakness, difficulty breathing and other issues. The most common type causes mild symptoms.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Osteogenesis imperfecta (OI) is a connective tissue disease. It makes your bones fragile. You might break a bone with little or no force. That’s why OI is also known as brittle bone disease. It makes your bones weaker and thinner than they should be.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Osteogenesis imperfecta also affects your body’s ability to make collagen properly. Collagen is a protein. It helps develop your:
Osteogenesis imperfecta can cause many broken bones throughout your life. It can also affect your:
The most common form of osteogenesis imperfecta usually causes mild symptoms. But OI can also cause severe disabilities and be fatal.
Healthcare providers classify osteogenesis imperfecta into 19 types. Types I through IV are the most common.
People with type I have lower amounts of normal collagen than they should. People with types II, III and IV have improperly formed collagen. These types cause more severe symptoms.
This is the most common form of OI. It causes milder symptoms than other types. You’ll break bones more easily than usual. But most broken bones happen before puberty. It doesn’t cause bone deformity.
Type II is the most serious form. Babies with type II die at or shortly after birth. It causes fatal complications like:
Type III is the second most severe form. It causes dangerous bone deformities. This makes your bones very fragile. You’ll live with physical disabilities. Babies with type III are often born with broken bones.
Advertisement
Type IV is more severe than type I. But it’s less severe than type III. Your bones will be more fragile than usual. But they won’t break as often as with type III.
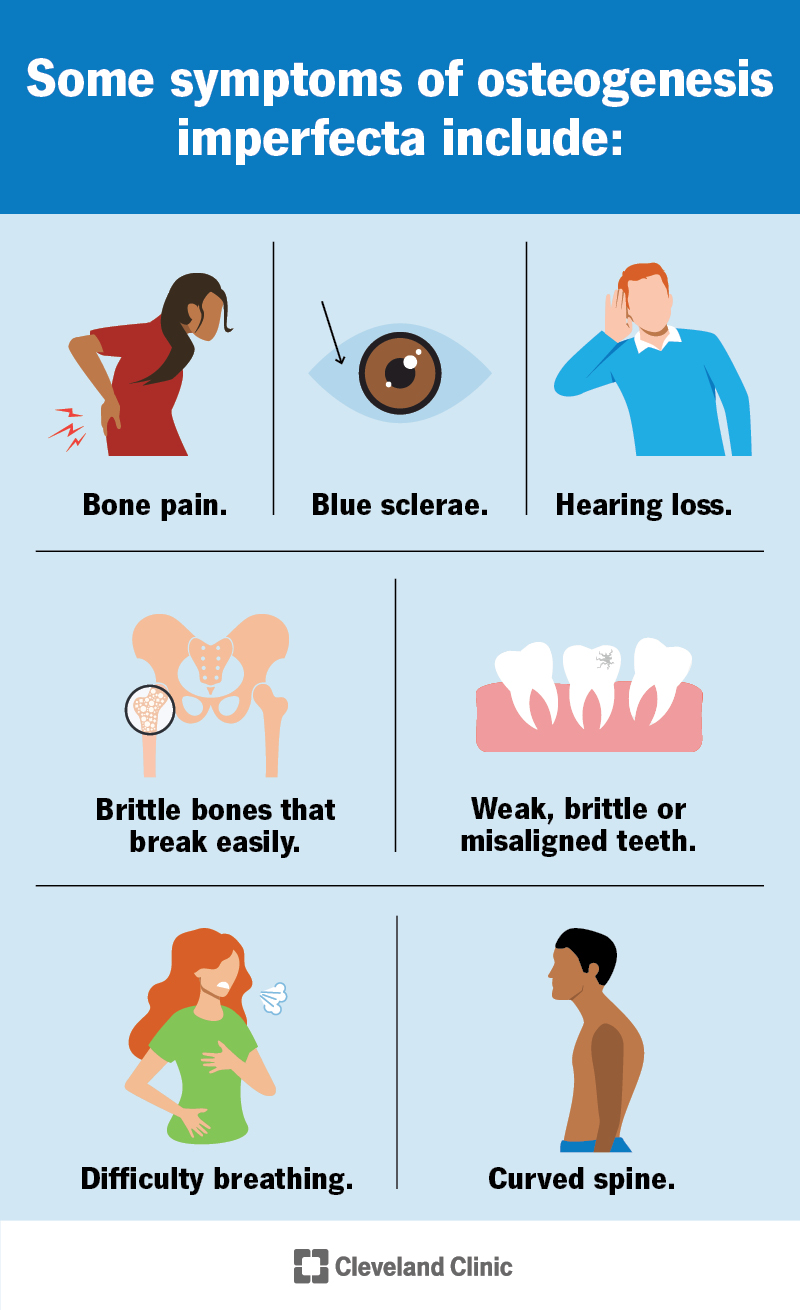
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/osteogenesis-imperfecta)
Signs and symptoms of this condition can include bone issues like:
You might also experience:
A genetic change causes this condition. Changes in the COL1A1 or COL1A2 genes cause most cases. Changes in other collagen genes cause rarer types of OI.
The genetic changes that cause OI can be random. You may also inherit them from your biological parents. You’re more likely to have OI if someone else in your biological family has it. Some people have the genetic variation but never develop osteogenesis imperfecta.
You can inherit the gene change from one parent (dominant) or both (recessive), depending on the type of OI.
Complications of osteogenesis imperfecta can include:
Healthcare providers usually diagnose brittle bone disease in childhood with:
A pregnancy care provider might suspect osteogenesis imperfecta before birth. They may see signs of OI on ultrasound images. They can confirm the diagnosis during pregnancy with an amniocentesis. They can also diagnose it after the baby is born.
Ask your provider about genetic counseling. This can help you understand your risk of passing osteogenesis imperfecta to your biological children.
Treatment for osteogenesis imperfecta can increase your bone strength. It can also help you live more independently. You might need:
Talk to a healthcare provider if you think you or your child has symptoms of OI. Tell your provider if you break bones easily. Especially without a major injury. Your provider can recommend additional testing if needed.
Advertisement
Go to the emergency room if you or your child breaks a bone. Tell providers in the ER if you know you have osteogenesis imperfecta.
Mild forms of osteogenesis imperfecta usually won’t affect your lifespan. But life expectancy varies depending on the type.
Because brittle bone disease is a genetic condition, you can’t prevent it. If you or your partner has OI or if you have a relative with the condition, you can talk to a genetic counselor. They can advise you about the risks of passing on the condition.
Learning that your child has a condition that’ll affect them for their whole life can feel overwhelming. The future might look much different from what you expected. But early occupational and physical therapy can help both you and your child adapt to these changes.
It can also help to have honest conversations with your child’s healthcare team and your loved ones every step of the way. They can help you make a plan to manage symptoms and prepare for the future.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When you have an inflammatory or autoimmune condition, you need experts by your side. At Cleveland Clinic, we’ll create an individualized treatment plan for you.
