Amniocentesis is a prenatal test that can diagnose genetic disorders (like Down syndrome and spina bifida) and other health issues in a fetus. A provider uses a needle to remove a small amount of amniotic fluid from inside your uterus. Then, a lab tests the sample for specific conditions.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
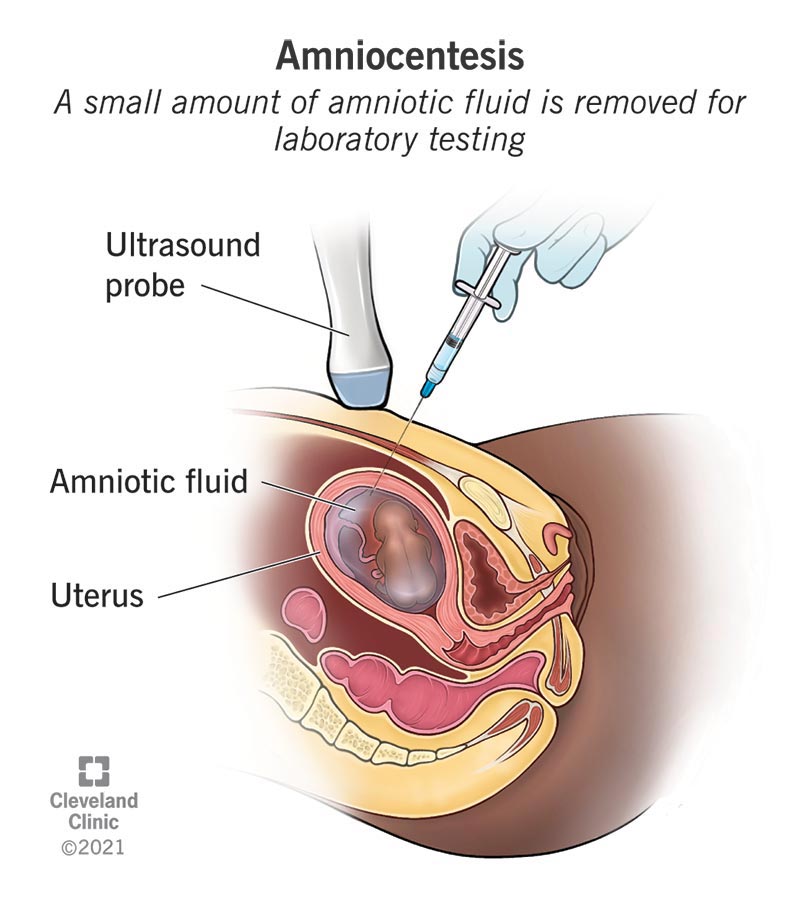
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/4206-genetic-amniocentesis)
Amniocentesis is a test that diagnoses certain congenital disorders and genetic conditions in a fetus before birth. During amniocentesis, your healthcare provider uses a thin needle to remove a small amount of amniotic fluid from the amniotic sac. This fluid sample is sent to a lab for testing.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The test usually happens between 15 and 20 weeks of pregnancy (during the second trimester). In some cases, it happens in the third trimester.
Your healthcare provider may recommend amniocentesis when:
Amniocentesis is completely optional. If your provider recommends you have the test, they’ll explain why. They can also discuss the benefits and risks with you.
An amniocentesis test can detect:
This test can also check:
Amniocentesis is also a treatment for polyhydramnios (when you have too much amniotic fluid). Providers use it to remove some of the excess amniotic fluid.
Advertisement
Amniocentesis can tell your pregnancy care provider if your baby will be born with a congenital or genetic disorder. Amniotic fluid contains some of the fetus’s cells. These cells contain genetic material that providers can test for certain conditions. During amniocentesis, your healthcare provider inserts a thin needle through your belly and into your uterus to get the fluid.
There usually isn’t anything special you have to do to prepare. Tell your provider what medications you’re taking so they can let you know if you should stop taking them.
It’s normal to have questions about the test. Some questions for your provider could include:
A perinatologist usually performs amniocentesis. First, you’ll lie back on an exam table with your belly showing. Then, they’ll:
After the procedure, your healthcare provider sends the sample to a lab. The lab separates the fetal cells from the amniotic fluid. The cells grow for several days in the lab. Then, they test the cells for genetic conditions or neural tube defects.
An amniocentesis procedure may take around 30 minutes from start to finish. But the sampling process (when the needle is inside you) takes only a minute or two.
You may be uncomfortable or feel a sting when your healthcare provider inserts the needle through your skin. You may also have minor cramping during the procedure. Cramps can last for a few hours after.
Amniocentesis is safe, but there are some risks. Some possible complications are:
Complications from amniocentesis are rare. About 1 or 2 in 100 women have spotting or cramping after amniocentesis. In about 1 in 1,000 cases, amniocentesis leads to miscarriage. Talk to your pregnancy care provider about the risks and benefits of the test.
It’s about 99% accurate. But it can’t tell you how severe the condition is, only that the fetus has the condition.
You should go home and relax for the rest of the day. You can take acetaminophen for any discomfort. Avoid any activity that takes a lot of physical effort, like exercise or sex. You should feel ready to get back to your typical routine in one or two days.
Advertisement
The time it takes to receive your results will depend on what conditions they’re testing for. You may hear from your provider as soon as three or four days after your test. Some test results may take two weeks or longer.
If your results are normal, it means there weren’t any signs of the conditions the test looked for.
If amniocentesis shows that the fetus has a condition, your healthcare provider can explain what that means. Genetic counseling may be available to help you understand what your options are moving forward and what you can expect.
You may also see a neonatologist. They can discuss specific treatments, surgeries or medications you may need. They can also talk about what kind of care your baby needs during the first days, months or years of life.
After an amniocentesis, call your provider if you have:
It’s normal to be nervous about a needle going into your belly during pregnancy. Healthcare providers perform amniocentesis tests for different reasons. They typically recommend amniocentesis when they believe the benefits of testing outweigh the small (but real) risks to you and your baby. But you get to make the final decision on whether having an amniocentesis test is right for you. Don’t be afraid to talk to your healthcare provider about your concerns. There’s no wrong answer.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Prenatal tests can give your providers information about your pregnancy and fetal development. Cleveland Clinic’s experts can guide you through prenatal testing.
