Open-angle glaucoma is an eye disease that causes slow, symptomless vision loss. You might not notice it until irreversible damage has been done. Fortunately, once you’ve discovered it, you can treat it, preventing further vision loss. Treatments include eye drop medications and surgery, which may be minimally invasive.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
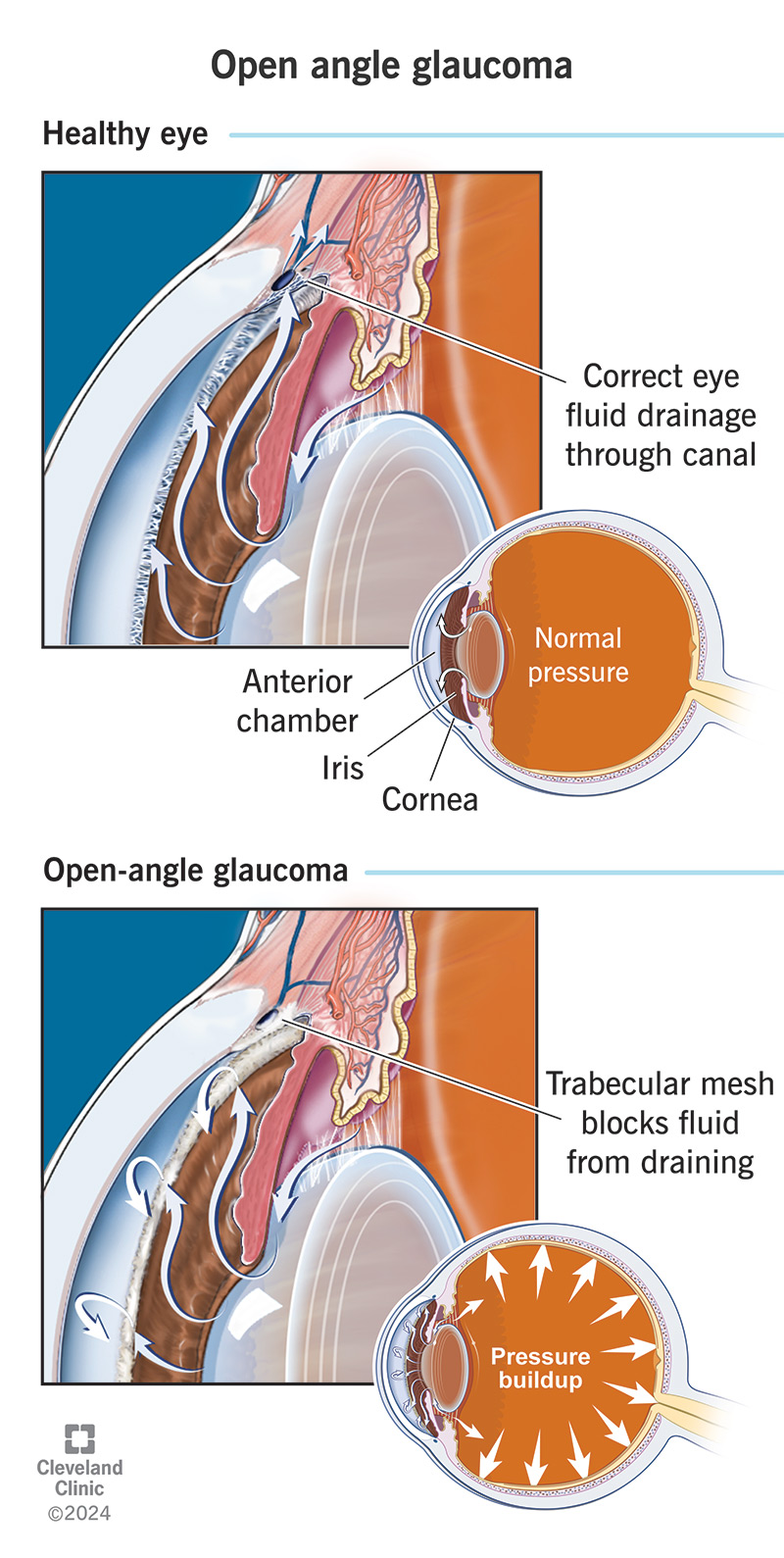
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/open-angle-glaucoma)
Open-angle glaucoma (OAG) is the most common type of glaucoma— an eye disease that damages the optic nerve in your eye. In open-angle glaucoma, your eye’s drainage system starts to back up — usually, so slowly that you don’t notice. This prevents your eye fluids from draining normally. As fluids build up, they raise the pressure inside your eye, causing ocular hypertension. This damages your optic nerve.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
OAG is a sneaky condition that starts without any obvious symptoms or causes and continues to worsen, causing gradual vision loss. You might not realize it’s happening until your vision is significantly impaired. This damage is irreversible. Treatment focuses on improving drainage and reducing the pressure in your eyes to stop the condition from progressing. Without treatment, OAG can progress to blindness.
Vision loss from open-angle glaucoma starts at the edges of your visual field (your peripheral vision) and slowly closes in on the center. Most people have vision loss in both eyes, but it’s usually more advanced in one eye. This makes it harder to notice, because the stronger eye compensates for the weaker one.
Most people don’t notice symptoms until they have significant vision loss.
Signs might include:
You or your eye care provider may also notice specific visual field defects during testing, like:
Advertisement
As OAG advances, it leads to gradually worsening tunnel vision.
Open-angle glaucoma progresses slowly, but surely. It’s serious because it can affect your vision before you realize it. With treatment, you can stop or slow the progression. But without it, it can lead to low vision or blindness. Vision loss from OAG is usually painless. But some people develop a complication called retinal venous occlusion that causes eye pain with blindness. This can be more difficult to treat.
Your eyes have a built-in drainage system for the fluid that they produce. Glaucoma happens when something interferes with this drainage system and the fluid builds up inside. As this happens, it raises the pressure inside your eye. If your eye has elevated pressure for a long period of time, it can damage your optic nerve. This is the nerve that carries messages from your eye to your brain so you can “see.”
Sometimes, the problem in your eye’s drainage system is clearly visible, and sometimes it isn’t. In open-angle glaucoma, your eye’s drainage angle appears to be open and functioning normally. But somehow, resistance seems to build up within it. Experts believe the issue is in the trabecular meshwork — a spongy tissue inside the drainage angle that fluids drain through. Most treatments target this tissue.
The problem is similar to what happens to the trabecular meshwork with aging. It loses cells, changes form and becomes less functional. It’s almost like something has sped up the aging process in these tissues. Most of the time, there’s no obvious reason for this. In this case, healthcare providers call it primary open-angle glaucoma. But sometimes, another condition causes it, and then it’s called secondary open-angle glaucoma.
In secondary OAG, another condition clogs the pipes in your eye drainage system. Examples include swelling, protein deposits or cellular debris. Primary OAG is harder to explain. There’s often evidence of ocular hypertension, but not always. Sometimes, the pressure in your eye can still be normal, but you still have signs of damage to your optic nerve. Certain risk factors may increase your risk of primary OAG, including:
It’s tricky to get a glaucoma diagnosis if you don’t notice symptoms or vision changes. Seeing your eye care specialist for regular eye exams can help catch it sooner. If your provider has a record of your previous exams and your eye health history, they’ll be more likely to notice small changes and risk factors that could suggest glaucoma. This could lead to further testing and an earlier diagnosis.
Advertisement
Specialists diagnose OAG when you have evidence of:
Tests to diagnose glaucoma may include:
Treatments for open-angle glaucoma include medications and procedures. Which treatment will work best for you will depend on your condition and how it responds. Most treatments aim to reduce the intraocular pressure (IOP) in your eye. Even if your IOP doesn’t seem especially high, studies show that reducing it slows the progression of glaucoma. This helps to preserve as much of your vision as possible.
Healthcare providers often start by prescribing medications to treat open-angle glaucoma. These are usually topical eye drops that either increase the outflow or decrease the production of the fluid building up in your eye. This reduces pressure. Don’t worry: this fluid (aqueous humor) is different from the tears that lubricate your eye. Adjusting these fluid levels won’t make your eyes too dry.
Common medications for OAG include:
Advertisement
Your eye care provider might recommend eye surgery for OAG if medications aren’t helping enough, or you don’t want to continue using them. In some cases, they might recommend minimally invasive surgery as a frontline treatment to avoid medications. There are many types of glaucoma surgery. Procedures for open-angle glaucoma tend to focus on improving drainage in the trabecular meshwork.
Common procedures for OAG include:
With treatment, most people can stop OAG from progressing, or at least slow it down. But the vision loss you have before you start treatment is irreversible. Without noticeable symptoms, some people don’t realize they’re slowly losing their vision until it’s too late. While most people won’t progress to blindness, glaucoma is the second-leading cause of blindness worldwide. And most glaucoma is OAG.
Advertisement
For unclear reasons, glaucoma affects people with African racial heritage more severely than others. African American, Afro-Caribbean and West African people are four times more likely to develop it. They tend to develop it decades younger, and they’re six times more likely to be diagnosed with advanced vision loss. After cataracts, glaucoma (usually, OAG) is the leading cause of blindness in Black people.
Most of the time, there’s no obvious cause for open-angle glaucoma, so there’s no way to prevent it. But catching it and treating it earlier can prevent some of the damage it does. The best way to do this is to see your eye care provider regularly for routine eye exams. If you have a higher risk of developing OAG, your provider might recommend more frequent testing, or in some cases, preventive treatment.
If you’re treating OAG with medications, it’s important to take them consistently. Unlike procedures, medications aren’t a long-term fix for OAG. You have to take them every day, possibly forever. This may be difficult if they cause symptoms or side effects, or if you don’t notice the difference when you stop. If your current treatment plan isn’t working, be sure to revisit your options with your provider.
Open-angle glaucoma, the most common type of glaucoma, develops slowly, without warning and often without symptoms. It can cause vision loss before you’ve had any reason to suspect it. This can be a heavy and bewildering diagnosis to receive. But once you’ve received it, you can begin to treat it. Many people successfully manage OAG with medications and/or with a minimally invasive procedure.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Glaucoma can cause vision loss if left untreated. Cleveland Clinic can quickly diagnose glaucoma and give you the ongoing expert treatment you need.
