Oculocutaneous albinism happens when DNA mutations disrupt how your body makes the pigment responsible for your skin, hair and eye color. This condition can also affect your sight. Many types of this condition exist, and there are several possible treatments that can help.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
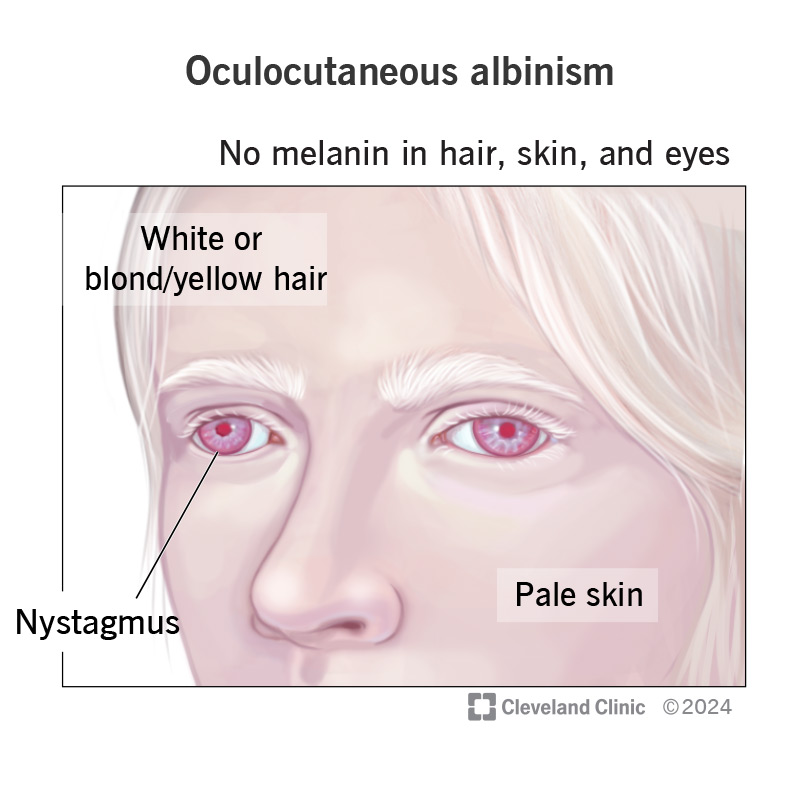
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/oculocutaneous-albinism)
Oculocutaneous albinism (OCA) is a rare genetic disorder that affects the color of your eyes, skin and hair. Having albinism means your body can’t produce and/or distribute a key pigment, melanin. Melanin is what gives your eyes, skin and hair their color, so your skin, hair and eyes may have much lighter coloration than expected. Not having enough melanin is also a major issue because your eyes need it to work correctly.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Because oculocutaneous albinism can affect your appearance, it’s understandable to feel self-conscious about having it. And some of the effects of OCA can disrupt how your eyes work. That can be frustrating or even frightening. But there are treatments that may help limit the eye symptoms and effects of this disease.
OCA has many possible symptoms you can experience or see. It also has several clinical signs, which are differences or changes that a trained medical professional can find with specific methods or tests.
The most visible symptoms of OCA are color differences in your hair and skin. People with oculocutaneous albinism often have:
Oculocutaneous albinism can cause very noticeable differences or changes in your eye color. If you have OCA, you may have light blue/pale gray irises. When light shines on your eyes, your irises may appear pink or red. These colors may also change during your lifetime. Brown irises are still possible with some subtypes of OCA.
Advertisement
Other possible, eye-specific signs of oculocutaneous albinism you might notice include:
There are other signs of OCA that your eye care provider may see during a vision exam. For example:
Some types of oculocutaneous albinism or conditions that can cause it can also cause other specific symptoms and effects. A few examples include:
Most of these other symptoms happen with rarer types of OCA. Your healthcare provider is the best source of information about the symptoms you (or a child you care for) may experience.
OCA happens when a gene (DNA) change (mutation) affects how melanin works in your body. So, it’s a genetic condition that’s either:
Melanin is a protective pigment. Your body makes it to absorb ultraviolet (UV) radiation from the sun, which is why sun/UV exposure causes tanning in people without albinism. UV rays damage the DNA in your skin cells. That damage increases your risk of those cells malfunctioning and turning into different forms of skin cancer, especially basal cell carcinoma and squamous cell carcinoma. And UV damage adds up, so the more damage you have, the greater your chances of developing cancer.
A healthcare provider may suspect oculocutaneous albinism because of visible differences in the color of your skin, hair or eyes. This often happens very early in life, with pediatricians or other child-focused providers doing the initial work to diagnose this condition. Healthcare providers can use a combination of methods to confirm and diagnose OCA, including the specific type and subtype you have.
Advertisement
Methods that may play a role in diagnosing oculocutaneous albinism include:
There’s no cure for oculocutaneous albinism, but there are a few treatments that might help.
For people with OCA, a key focus is treating related eye conditions, including:
Your eye specialist will also likely recommended sunglasses or tinted lenses to help with light sensitivity and protect your eyes from sun exposure.
One medication, nitisinone (Nityr® or Orfadin®), may help people with oculocutaneous albinism type-1. Nitisinone slows how your body breaks down tyrosine, a key amino acid. A research study published in 2019 showed nitisinone helped with pigmentation and eyesight in a group of five adults with oculocutaneous albinism type-1. Researchers also suspect that giving nitisinone earlier in life to people with oculocutaneous albinism type-1 might have even bigger benefits.
Because there are so many variables that can play a role in treatment, your eye care specialist is the best source of information about possible treatments. They can guide and advise you as you choose treatments that will help you (or a child you care for).
Advertisement
Oculocutaneous albinism is a lifelong disorder that can have a wide range of effects. Most people with OCA will have visible differences in their eyes, hair and/or skin. But those differences can vary. Some people will have differences that stand out, but not everyone with oculocutaneous albinism does.
Most people with OCA will have various related health concerns, especially eye issues, but it’s rare for oculocutaneous albinism to cause dangerous or life-threatening issues on its own. The most important complication to avoid is skin damage from the sun or other sources of UV rays.
With regular medical and vision care, most people with oculocutaneous albinism can expect a life like those who don’t have OCA. This disorder usually doesn’t affect your life expectancy, especially if you avoid skin cancer-related complications.
Oculocutaneous albinism (OCA) can be a condition that’s easy to see, or it can be a condition that doesn’t cause effects that are easily visible to others. Living with this condition — visible or invisible — can come with challenges. But these are challenges that you can seek help for. If you or a child you care for has symptoms of oculocutaneous albinism, it’s a good idea to see a healthcare provider or eye care specialist. They can help guide you in getting a diagnosis and finding treatment options and resources that may help.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s primary care providers offer lifelong medical care. From sinus infections and high blood pressure to preventive screening, we’re here for you.
