Stiff person syndrome is a rare, chronic condition that causes muscle stiffness and painful muscle spasms. The severity of symptoms varies from person to person. There’s no cure for stiff person syndrome, but treatment can help manage symptoms and slow the progression of the condition.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Stiff person syndrome (SPS) is a rare autoimmune neurological disorder that causes muscle stiffness in your trunk and abdomen (the middle part of your body). Over time, you may also develop stiffness (rigidity) and spasms in your legs and other muscles. Walking may be difficult, and you may become more prone to falls and injury.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Understanding and managing your stiff person syndrome diagnosis can be overwhelming. Your healthcare team will create a treatment plan that’s unique to you and your symptoms, as they vary from person to person. It’s important to make sure you’re getting the support you need to stay healthy by scheduling regular visits with your providers throughout your life.
Stiff person syndrome used to be called “stiff man syndrome,” but the name was updated to reflect that it can affect anyone, regardless of age or sex.
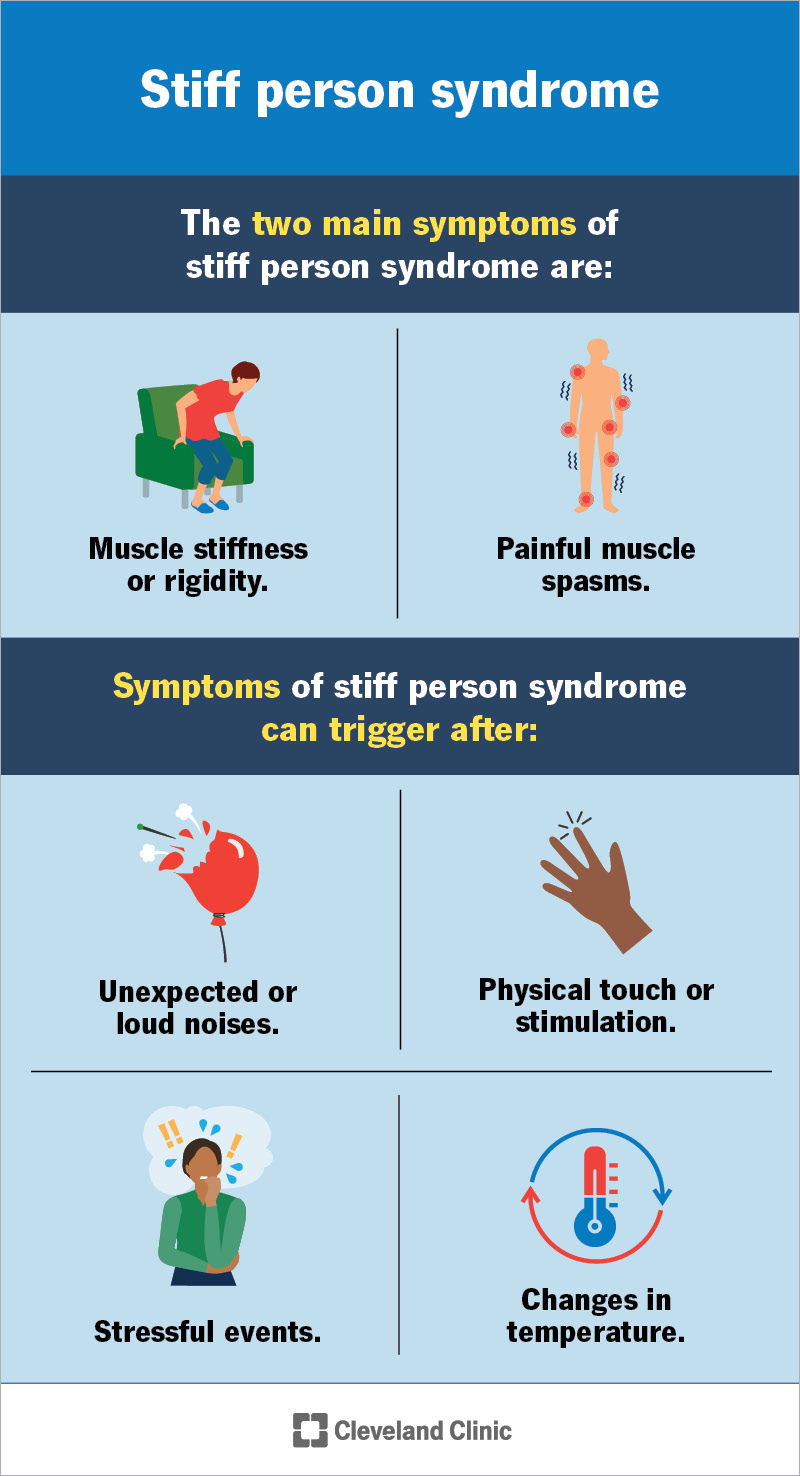
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/6076-stiff-person-syndrome)
The two main symptoms of stiff person syndrome are:
Symptoms can develop at any age, but they most often begin in your 30s and 40s.
Stiff person syndrome symptoms can spread to other areas of your body and/or get worse over time. Symptoms can take several months to a few years to develop. Some people’s symptoms remain the same for years. Others experience slowly worsening symptoms, including more severe spasticity/rigidity, which can limit their ability to perform activities of daily living.
In most cases of stiff person syndrome, the first symptom you’ll experience is muscle stiffness in your trunk (abdomen, chest and back muscles). The rigidity causes pain and an aching discomfort. These symptoms can fluctuate (swing) in severity without a clear reason or trigger. They can also affect your arms and legs. As stiffness increases, some people develop an abnormal posture that can make it difficult to walk or move.
Advertisement
Painful muscle spasms are another symptom of stiff person syndrome. They can involve your entire body or only a specific area. These spasms can last a few seconds, minutes or, occasionally, a few hours.
Symptoms of stiff person syndrome, like muscle spasms, can trigger (happen) after:
Due to the unpredictable triggers of muscle spasms, some people with SPS develop anxiety and agoraphobia — an extreme fear of entering open or crowded places or of leaving their homes. This is because it’s more difficult to avoid the triggers of muscle spasms out in public.
Researchers don’t know the exact cause of stiff person syndrome. But they think it’s an autoimmune condition. This is a condition in which your immune system attacks healthy cells for unknown reasons.
Studies suggest antibodies may play a role in SPS. Many people with stiff person syndrome make antibodies against glutamic acid decarboxylase (GAD). GAD makes a neurotransmitter called gamma-aminobutyric acid (GABA), which helps control muscle movement.
Researchers don’t yet understand the exact role that GAD plays in the development and worsening of stiff person syndrome. It’s important to note that the presence of GAD antibodies doesn’t mean that you have stiff person syndrome. In fact, a small portion of the general population has GAD antibodies without any adverse effects.
There are other antibodies associated with stiff person syndrome, including glycine receptor, amphiphysin and DPPX (dipeptidyl peptidase-like protein 6) antibodies. There are also some people with this condition who have no detectable known antibodies. Research is ongoing to discover if other potential antibodies may also cause symptoms.
Stiff person syndrome is twice as common in females. It may also happen with other autoimmune conditions, like:
Stiff person syndrome is very rare. About 1 out of every 1 million people have this condition.
A healthcare provider will diagnose stiff person syndrome by looking for specific signs of the condition with exams and testing. They’ll ask you questions about your symptoms during a physical exam and neurological exam.
If your provider suspects stiff person syndrome, they may offer tests, which could include:
Advertisement
Stiff person syndrome can be difficult to diagnose, as it’s rare and its symptoms are similar to other conditions, like ankylosing spondylitis, multiple sclerosis or other autoimmune conditions.
There are several different subtypes or classifications for stiff person syndrome, including:
The two main treatment strategies for stiff person syndrome include:
Treatment for stiff person syndrome varies based on your symptoms. Treatment aims to manage how symptoms affect you and improve your mobility and comfort.
Advertisement
Your healthcare team may include several specialists, including:
Medications can help decrease stiffness, rigidity and painful muscle spasms, including:
Therapies that may also help manage symptoms include:
There’s some evidence to suggest that intravenous immunoglobulin (IVIg) treatment (a type of immunotherapy) can improve stiff person syndrome symptoms.
Advertisement
IVIg contains immunoglobulins (natural antibodies your immune system produces) donated by thousands of people with healthy immune systems.
There’s currently no cure for stiff person syndrome. Treatment can help you manage symptoms.
Stiff person syndrome is a chronic (lifelong) condition. The prognosis (outlook) varies from person to person based on a few factors, including:
Starting treatment soon after symptoms begin is essential to prevent or lessen the syndrome’s progression and avoid long-term complications. Most people with stiff person syndrome improve with medications, but it can still be difficult to manage triggers that cause muscle spasms.
Over time, walking can become more and more difficult. Your ability to perform daily routine tasks may also decline over time. The increased risk of falls also becomes a growing concern as the condition worsens. You may need to use a cane, walker or wheelchair for assistance.
As stiff person syndrome is an autoimmune-related condition, there isn’t anything you can do to prevent it.
If possible, try to find a healthcare provider who specializes in researching and treating stiff person syndrome. Because the syndrome is rare, this could be difficult. You may have to advocate for yourself to ensure you get the best medical care that can help you have the best quality of life.
It’s common for people with stiff person syndrome to experience anxiety or depression related to the condition. If you’re experiencing mental health symptoms, it’s important to talk to your provider or a mental health specialist, like a therapist or psychologist.
You and your family may also want to consider joining a support group to meet others who can relate to your experiences.
If you have stiff person syndrome, you’ll need to see your healthcare team regularly to check if your treatment is working and to monitor the progression of your symptoms.
If you notice new symptoms or side effects of your medications, talk to your provider.
If you have stiff person syndrome, it may help to ask your healthcare provider the following questions:
It isn’t easy learning that you have a rare condition like stiff person syndrome. You may feel overwhelmed and unsure of what your future may look like. But you don’t have to face this alone. Your care team will be with you to answer any questions and help you manage symptoms as they arise.
While your care may focus on your physical health, make sure to monitor your mental health as well. Symptoms affect each person differently. But living with pain, discomfort and unpredictable muscle spasms can take a toll on your emotional well-being. Stiff person syndrome may make going out in public or performing everyday tasks more difficult, so don’t hesitate to contact a healthcare provider in addition to loved ones if you need support.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
There are ways to manage the pain, rigidity and spasms that come with stiff person syndrome. Cleveland Clinic’s expert providers are here to help.
