Orthostatic hypotension is a large drop in blood pressure (more than 20 millimeters of mercury in the top number or 10 mmHg in the bottom number) that occurs when you stand up after sitting or lying down. This can make you feel dizzy or faint when your body can’t adjust your blood pressure quickly. Causes include dehydration or certain conditions.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
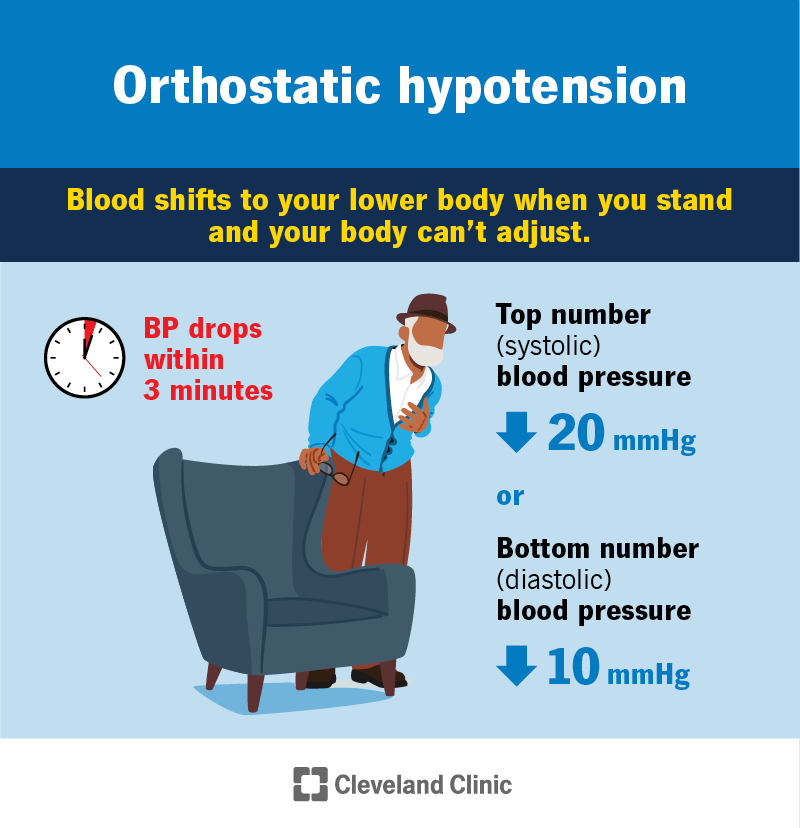
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/9385-orthostatic-hypotension-cv)
Orthostatic hypotension (postural hypotension) is a sudden drop in blood pressure when you stand after sitting or lying down. You may feel dizzy or even faint. This can happen for many reasons, like a loss of blood or fluids or a heart issue. Treating the causes improves symptoms.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
This condition affects many people over 60, especially those who live in long-term care residences. It’s also common among people who’ve been on bed rest or given birth recently. Teens having growth spurts can experience it as well.
Postural hypotension happens more frequently — and with more severe symptoms — in the morning. That’s because blood pressure is normally at its lowest when you wake up in the morning.
With orthostatic hypotension, your heart rate doesn’t increase. This makes it different from postural orthostatic tachycardia syndrome (POTS).
The main symptom of orthostatic hypotension is dizziness or lightheadedness when you stand. Some people faint. You should feel better when you sit or lie down.
Other orthostatic hypotension symptoms include:
Some people don’t have any orthostatic hypotension symptoms. Others find that hot temperatures (from the weather, a fever, or even a hot tub or shower) make symptoms worse.
This condition happens when your body can’t adjust to a large amount of blood moving to your lower body when you stand. This amount of blood could fill a large coffee cup or a water bottle.
Advertisement
When you’re sitting or lying down, blood from the veins in your legs flows easily to your heart. When you stand up, the blood in your legs and feet has a harder time reaching your heart. There’s less blood available for your heart to send to organs and muscles. As a result, your blood pressure briefly drops.
Postural hypotension causes may include:
Orthostatic hypotension becomes more common as you age. After 65, your body can’t manage blood pressure as well, and your arteries get stiff. But anyone can get this condition if they take certain medicines, have a heart condition, lose too much fluid or stand too long.
These factors increase your risk:
If you’re prone to postural hypotension, these steps can help reduce symptoms:
Advertisement
People with orthostatic hypotension may have a higher risk of:
Your healthcare provider will check your blood pressure while you’re sitting, lying down and standing. Healthcare providers diagnose this condition based on how low your blood pressure goes when you stand up. You meet the orthostatic hypotension criteria if your blood pressure drops more than 20 millimeters of mercury in systolic (top number) pressure or 10 mmHg in diastolic (bottom number) pressure within three minutes of standing up.
Your provider will examine you and ask questions about your medical history.
You may also get one or more of these tests:
Advertisement
Orthostatic hypotension treatments vary depending on what’s causing the condition. You may need to wear compression stockings, change a medication dose or take new medicine.
Treatments may include:
Rarely, people with postural hypotension need medications to increase blood volume and pressure. These medications include:
You should call a healthcare provider if you often get dizzy when you stand up. Contact them even if this only happens some of the time.
Get immediate treatment if you have:
You may want to ask your healthcare provider:
Advertisement
There’s no cure for orthostatic hypotension, but it rarely causes long-term problems. Most people with this condition can manage symptoms by:
Orthostatic hypotension symptoms can be unsettling. They may even be dangerous if you lose your balance, fall or pass out. Symptoms often improve when you change how you move into a standing position. Tell your healthcare provider about your symptoms. You may need to change your medications to reduce or prevent symptoms. In more severe cases, your provider may prescribe medicine to improve blood flow and pressure.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When your heart needs some help, the cardiology experts at Cleveland Clinic are here for you. We diagnose and treat the full spectrum of cardiovascular diseases.
