Athlete’s heart describes differences in your heart’s left ventricle and other changes that happen when you exert yourself for an hour a day on most days of the week. A provider can pick up unusual heart sounds through a stethoscope or testing. However, this is a harmless condition with no symptoms.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
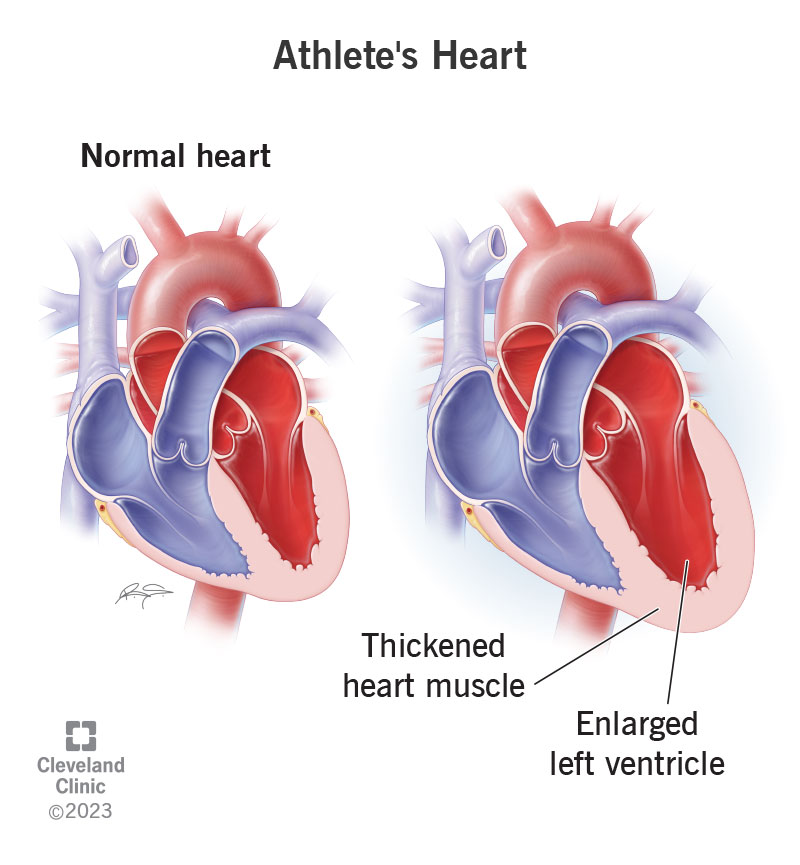
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/23920-athletes-heart)
Athlete’s heart is the name for the changes that happen in your heart when you do strenuous exercise for more than one hour on most days of the week. Most of the time, these changes aren’t excessive. However, in some athletes, the changes can make your heart look similar to how it looks when you have a form of cardiomyopathy. Because cardiomyopathy isn’t harmless, your provider needs to know what makes athlete’s heart different.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Some electrocardiogram results appear similar for these two conditions. It’s important to know the difference because one is dangerous and the other isn’t.
Athlete’s heart affects 2% of athletes. This can happen after years of strenuous training. Athlete’s heart is much more common in athletes who are Black than in people of other races.
Your body needs more oxygen when you exercise. To meet this higher demand, your heart’s left ventricle handles more blood and a higher pressure than normal. Your left ventricle pumps oxygen-rich blood to your aorta, which sends it out to your body.
After meeting your body’s need for more blood and oxygen for a while, your left ventricle starts to get bigger and develop thicker heart muscle.
When you’re not working out, your heart doesn’t have to pump as much blood. It can pump what you need at a lower heart rate. This is why people with athlete’s heart syndrome have a heart rate that’s lower than a non-athlete’s heart rate at rest.
Advertisement
There aren’t any athletic heart syndrome symptoms. You most likely have a different heart issue if you have chest pain or palpitations.
Intense endurance training or strength training can cause athletic heart syndrome in some athletes.
Endurance sports tend to increase the size and wall thickness of an athlete’s left ventricle.
Sports that can lead to athlete’s heart include:
A healthcare provider can diagnose you based on athlete’s heart syndrome signs and symptoms, such as:
Tests to diagnose athlete’s heart include:
You don’t need treatment for athlete’s heart syndrome. But your healthcare provider may ask you to stop training for three months and then reimage your heart to ensure you don’t have cardiomyopathy.
Yes. In most people, your heart returns to a normal size after you stop training so hard. However, a study found that 20% of former athletes still had a large left ventricle five years later.
Exercise is good for your heart, and people with an athletic heart don’t have problems from it later. A study of high-level athletes found that their endurance training didn’t cause heart issues in the future.
Athlete’s heart continues as long as you don’t ease up on your training. After three months without training, your heart goes back to normal.
Because athlete’s heart is the heart’s normal response to intense, aerobic exercise, you don’t need to reduce your risk because it’s not a dangerous condition.
Contact a healthcare provider if you have these symptoms:
While these aren’t linked to athlete’s heart, they could mean you have coronary artery disease or cardiomyopathy.
You should call 911 or emergency services if you think you may be having a heart attack. You should also call 911 if you see someone collapse and not respond.
If your healthcare provider thinks you may have a type of cardiomyopathy instead of athlete’s heart, they may ask you to stop training so they can be sure. If this happens, ask them if there are other tests they haven’t tried yet. If they’ve done all the tests they can but still suspect you may have cardiomyopathy, it can be tough to give up training to see if your heart goes back to normal. Consider your health and your future. Talk with your provider about it. Sports may be important to you, but your life is, too.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When your heart needs some help, the cardiology experts at Cleveland Clinic are here for you. We diagnose and treat the full spectrum of cardiovascular diseases.
