Duchenne muscular dystrophy (DMD) is a condition that causes skeletal and heart muscle weakness that quickly gets worse with time. Symptoms usually begin by age 6. The disease mainly affects boys. There currently isn’t a cure. Treatment involves managing symptoms and improving quality of life.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Duchenne muscular dystrophy (DMD) is a progressive condition that causes muscles to get weaker over time. It mainly affects the muscles used for movement, breathing and heart function.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
It’s inherited and it typically affects males. Symptoms usually start in early childhood and slowly get worse. You might notice developmental delays, toe walking or muscle weakness in your child as they grow.
This disease affects about 1 in every 3,600 male infants. It’s the most common form of muscular dystrophy and the leading type of severe inherited muscle disorder (myopathies).
While there’s no cure, and it will shorten life expectancy, treatments are available to slow its progression and help your child manage symptoms.
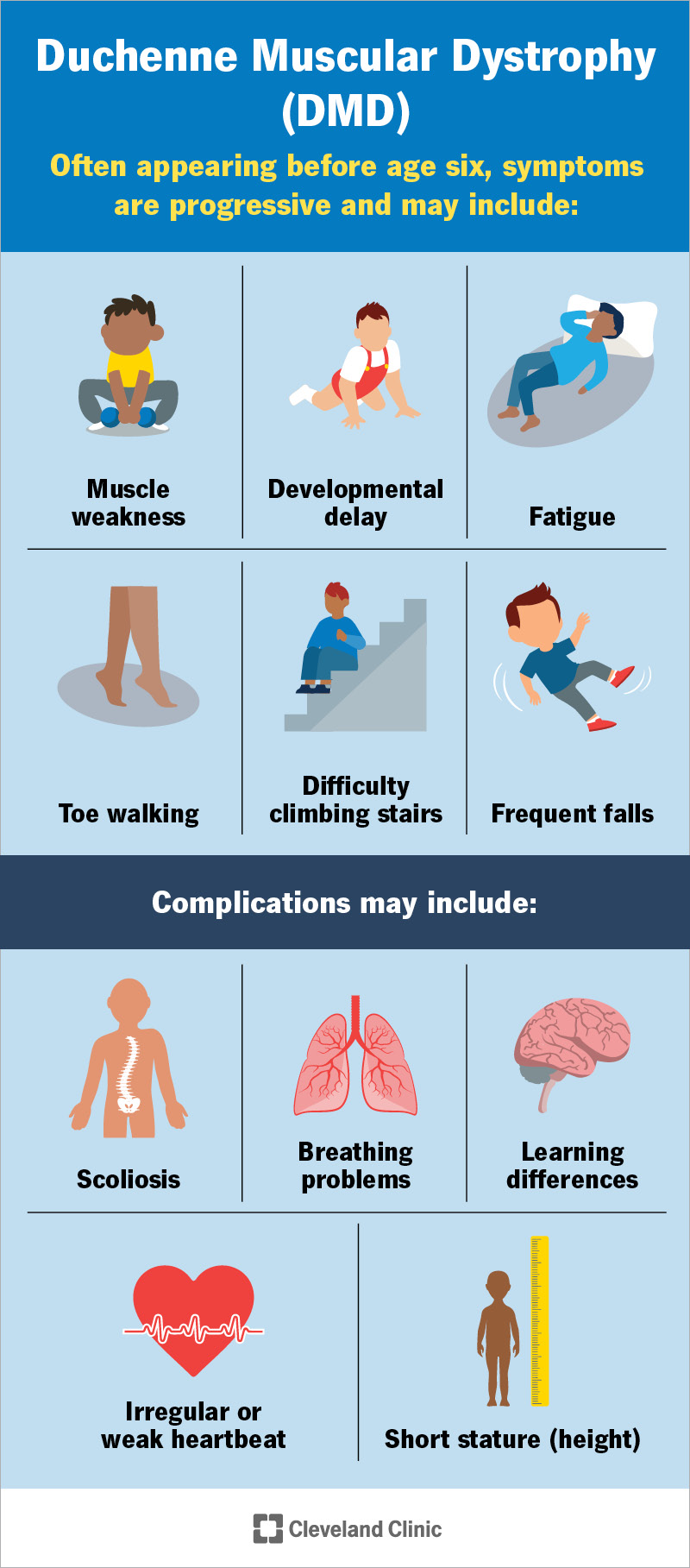
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/23538-duchenne-muscular-dystrophy)
DMD symptoms worsen over time and may include:
Muscle weakness can affect how your child walks and moves. You might notice these signs:
Symptoms of DMD usually appear between the ages of 2 and 4. They can start as early as infancy, but you might not notice them until later in childhood.
A genetic variant causes Duchenne muscular dystrophy. This gene tells their body how to make a protein called dystrophin. Dystrophin keeps muscles strong and protects them when they move.
Advertisement
If your child has this condition, their body makes little or no dystrophin. Without it, their muscles become weak and start to break down. Over time, muscle cells die, and their body can’t replace them. Instead, the empty spaces fill with fat and scar tissue. This makes movement even harder.
DMD is usually passed down through families. It’s X-linked recessive. Here’s how that works.
The gene that causes it is on the X chromosome. This is one of the two sex chromosomes:
As boys only have one X chromosome, if that X chromosome has the gene change that causes DMD, they’ll have the disease. This is because they have no backup copy on another X chromosome to make up for it. Girls, on the other hand, have a backup copy on their other X chromosome and typically won’t be affected.
Girls either don’t have symptoms or they’re very mild. Girls may become carriers. Carriers inherit the gene change but don’t have symptoms. They may pass the gene on to their future children.
However, in about 3 out of 10 cases, the gene change happens randomly. This means it wasn't passed down and there wasn’t a family history. There’s no way to prevent Duchenne muscular dystrophy.
If your child shows signs, see their pediatrician. Their provider will do a physical, neurological and muscle exam. They’ll also ask about your child’s symptoms and medical history.
If they think it’s DMD, their provider may refer you to a pediatric neurologist or order these tests to confirm a diagnosis:
There’s currently no cure for DMD. The main goal of treatment is to manage symptoms and slow progression. Supportive therapies may include:
Advertisement
If your child has this condition, they’ll need regular visits with their care team to manage treatment and track symptoms. You’ll get to know their providers well, as ongoing care is essential. As your child grows and their symptoms change, their treatment plan may need to adjust, too.
This disease is progressive despite treatment. That means it gets worse over time. The outlook is poor, as it shortens your child’s lifespan.
You can expect that your child will need to use a wheelchair by their 12th birthday. But this loss of mobility shouldn’t take away from their ability to play and enjoy childhood moments.
People with this condition typically live into early adulthood, though life expectancy varies. Advances in treatment and supportive care have helped many live longer than once expected.
Most face complications related to their heart or breathing. In some cases, issues like pneumonia or airway blockages can also become serious.
Learning that your child has Duchenne muscular dystrophy (DMD) is incredibly difficult. It’s a life-changing diagnosis, and it’s OK to feel overwhelmed.
While DMD will bring challenges, it doesn’t take away their ability to be a kid. They can still splash in the pool, play with friends and tell silly jokes. They’ll grow, learn and find their own way to thrive. And you’ll be right beside them.
Advertisement
As you care for your child, remember to care for yourself, too. Talking with a mental health professional or connecting with others through a support group can make a difference. If you have any questions about your child’s condition or how to get yourself support, talk to a provider.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have a neurological condition, you want expert advice. At Cleveland Clinic, we’ll work to create a treatment plan that’s right for you.
