Keratoconjunctivitis is the term for inflammation of your cornea (keratitis) and your conjunctiva (conjunctivitis). These are the clear tissues that cover the surface of your eye. If both are inflamed at the same time, something is seriously irritating your eye. See your healthcare provider right away.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
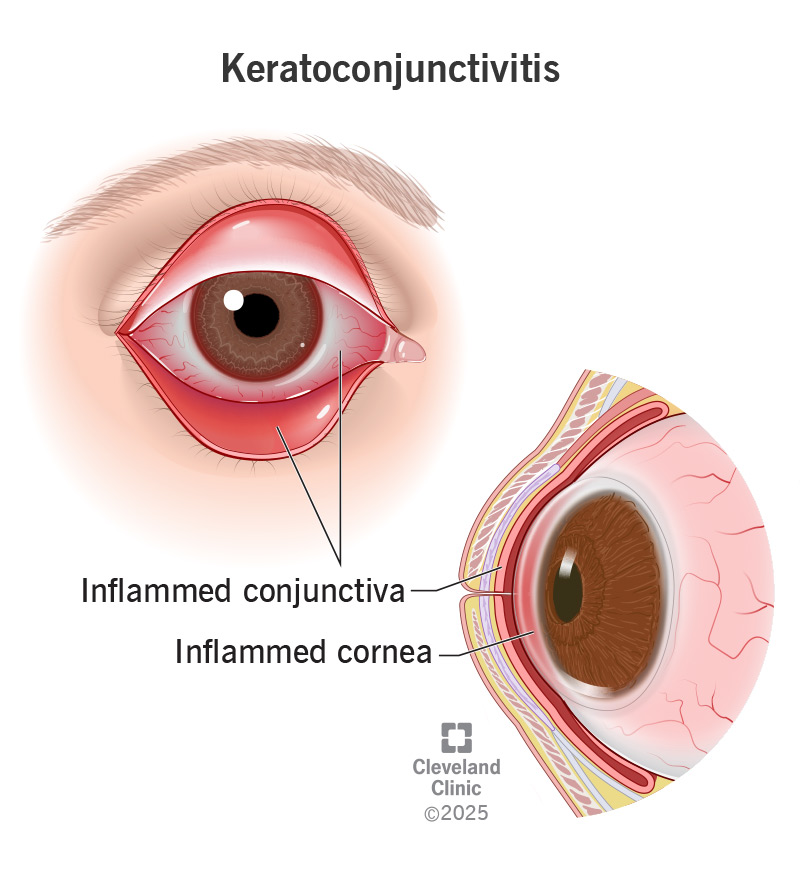
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/keratoconjunctivitis)
Keratoconjunctivitis is inflammation of the outer layer of your eyeball. It can happen when an infection, allergen or other irritant gets into your eye. There are also some other, less common causes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Specifically, keratoconjunctivitis means that two different parts of your outer eyeball are inflamed. Keratitis is inflammation in your cornea. That’s the clear window that covers your iris and pupil (the colored parts of your eye). Conjunctivitis is inflammation in your conjunctiva. That’s the clear film that covers your sclera (the white part of your eye). You may know conjunctivitis by its other name, pink eye.
Keratoconjunctivitis means you have both keratitis and conjunctivitis. So, whatever’s irritating your eye is affecting the whole surface of your eyeball. This might mean it’s more severe than usual.
Keratoconjunctivitis has many causes, some of which have their own names. You could consider these subtypes of keratoconjunctivitis. For example:
Advertisement
Signs and symptoms of keratoconjunctivitis may include:
Keratoconjunctivitis is inflammation in your cornea and conjunctiva. Inflammation in any part of your body is a reaction from your immune system. It’s reacting to something that it perceives as a threat.
Many things can trigger keratoconjunctivitis, including eye infections, allergies and autoimmune diseases. Some possible causes include:
Your eye care provider will start by reviewing your symptoms and medical history. They’ll ask you about your health conditions and any recent illnesses. Your provider may also perform various tests, including:
Treating keratoconjunctivitis depends on the cause. Some treatments include:
For very severe conditions, some people might need eye surgery.
See your healthcare provider if your eyes are red and irritated. See them right away if you have any unusual discharge or vision changes. Some causes of keratoconjunctivitis are more serious than others.
You might want to ask your provider:
Advertisement
Your prognosis depends on the type of keratoconjunctivitis you have. Some types clear up quickly with the right treatment. Others are chronic conditions that may come and go throughout your life. For these types, you may need regular treatment to manage your symptoms.
Treatment for keratoconjunctivitis is usually effective. It can help soothe the inflammation and can often address the underlying cause. But severe keratoconjunctivitis can do permanent damage to your eyes. So, it’s important to get treatment when you need it.
You can reduce your risk of keratoconjunctivitis by taking good care of your eyes. For example:
If your eyes are itchy and sore, or red where they should be white, contact your eye care specialist for an eye exam. Inflammation can damage your delicate eye tissues, even if it’s a common experience for you. Whether it’s seasonal allergies, an infection or something rarer, it’s important for your provider to isolate the cause so they can determine the best treatment for you.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s ophthalmologists and optometrists have the highest training available. We provide exams, vision correction and care for many eye conditions.
