Uterine sarcoma is a rare type of cancer that forms in the muscle or connective tissues of your uterus. The most common symptom is abnormal vaginal bleeding. Surgery is the go-to treatment, but you may need other therapies, like radiation or chemotherapy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
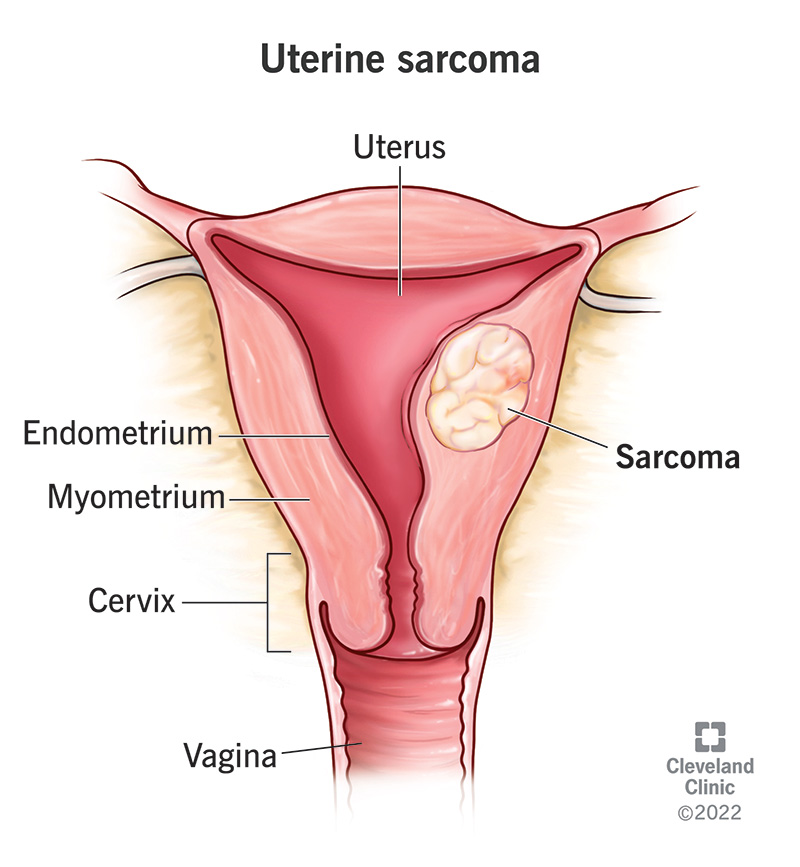
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/16408-uterine-sarcoma)
Uterine sarcoma is a type of uterine cancer that typically forms in the muscle layer of your uterus (myometrium). It’s rare, making up 2% to 5% of all uterine cancers.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Sarcomas are cancers (tumors) that start from tissues like muscle, bone and connective tissue. Cancers that start in epithelial cells, which line most organs, are called carcinomas. Most uterine cancer cases are carcinomas, not sarcomas.
Types of uterine sarcomas include:
In general, stages of uterine sarcoma include:
Advertisement
Cancer staging is complex. Healthcare providers use more specific stages, like stage IB or IIIA, for uterine sarcoma. Your team will explain the cancer stage in detail and what it means for you.
Symptoms of uterine sarcoma may include:
The main symptoms of uterine sarcoma are similar to uterine carcinoma and noncancerous growths, like fibroids. That’s why it’s important to see a provider if you notice any of these signs. The sooner you get a diagnosis, the better.
You may not notice symptoms until the uterine sarcoma has progressed to a more advanced stage. In rare cases, you may not have any symptoms (be asymptomatic).
Uterine sarcoma develops when immature uterine muscle or connective tissue cells have genetic mutations. The mutations cause the cells to develop into cancer cells that grow out of control.
Scientists don’t know exactly what triggers the DNA changes that lead to uterine sarcomas. They continue to research how to diagnose, treat and prevent them.
Factors that may increase your risk of developing uterine sarcoma include:
Black women are twice as likely as white women to develop uterine sarcomas. Researchers aren’t sure why race is a risk factor for this cancer.
Your healthcare provider will ask about your symptoms and medical history. They’ll also do a physical exam and pelvic exam.
They may recommend the following procedures:
A pathologist can confirm a diagnosis by examining cells with a microscope after a biopsy.
Advertisement
You may need additional tests to stage the cancer once you have a diagnosis. Imaging tests can reveal if the cancer has spread to other parts of your body (metastasized).
Your provider may refer you to a gynecologist who specializes in cancer (gynecological oncologist) to help with both diagnosis and treatment.
Receiving a cancer diagnosis can be overwhelming. It may be helpful to ask your healthcare team:
Surgery is the standard treatment regardless of the cancer grade. Types of surgeries include:
Advertisement
Your healthcare team may recommend other therapies to help treat uterine sarcoma, like:
Each type of therapy has potential risks and side effects. Your healthcare team will go over all of your options and what to expect. Together, you’ll decide on a plan that’s best for you.
Uterine sarcoma can be curable if it’s low-grade (mildly abnormal cells) and hasn’t spread beyond your uterus.
Uterine sarcoma is more difficult to treat than other uterine cancers. Still, the prognosis for uterine sarcoma depends on:
Talk to your healthcare team about your prognosis based on your unique case.
There’s no way to know for sure how long a person with uterine sarcoma will live. Each person’s outcome depends on several factors.
According to the National Cancer Institute, the survival rate for uterine sarcomas five years post-diagnosis ranges from 12% to 99.5%, depending on the type, grade and how much it’s spread. Talk to your healthcare team for more information.
Uterine sarcoma typically grows faster and spreads more quickly than more common uterine cancers. Still, not all uterine sarcomas are equally aggressive. Your provider will consider its location and type to determine how aggressive it is.
Advertisement
Your provider can also stage the cancer to see if it has spread.
A cancer diagnosis — especially a rare one like uterine sarcoma — can cause a flood of different emotions. The volume of new information can be overwhelming. An important thing to remember is that statistics can’t tell you how your treatment will go or what decisions are right for your specific situation. But your healthcare team will be by your side every step of the way. They’ll tailor your treatment to meet your needs and goals. Lean on loved ones for support, too.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic healthcare providers personalize uterine sarcoma treatment to your unique diagnosis and needs.
