Noncardiac chest pain is chronic pain that feels like angina, but it isn’t. Instead of your heart, it might be related to your esophagus, which runs close beside it. GERD and other esophageal disorders are common causes of noncardiac chest pain. Psychological conditions can also contribute.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Noncardiac chest pain (NCCP) is frequent, recurring pain in your chest that’s not related to your heart. It feels and behaves like cardiac chest pain (angina), but it isn’t. Healthcare providers diagnose noncardiac chest pain after ruling out heart-related causes. It’s often related to your esophagus (food pipe) instead.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Inside your chest cavity, your esophagus runs right alongside your heart. The same sensory nerves send pain signals from both organs to your brain. So, it may be hard to tell exactly where the sensations are coming from. It’s no coincidence that what we call “heartburn” is actually acid reflux in your esophagus.
Most people who experience chest pain don’t have heart disease. But it can be hard to tell if your chest pain is from heartburn or a heart attack, or something else. That’s why it’s important to seek care for chest pain. A qualified healthcare provider can determine if you have cardiac or noncardiac chest pain.
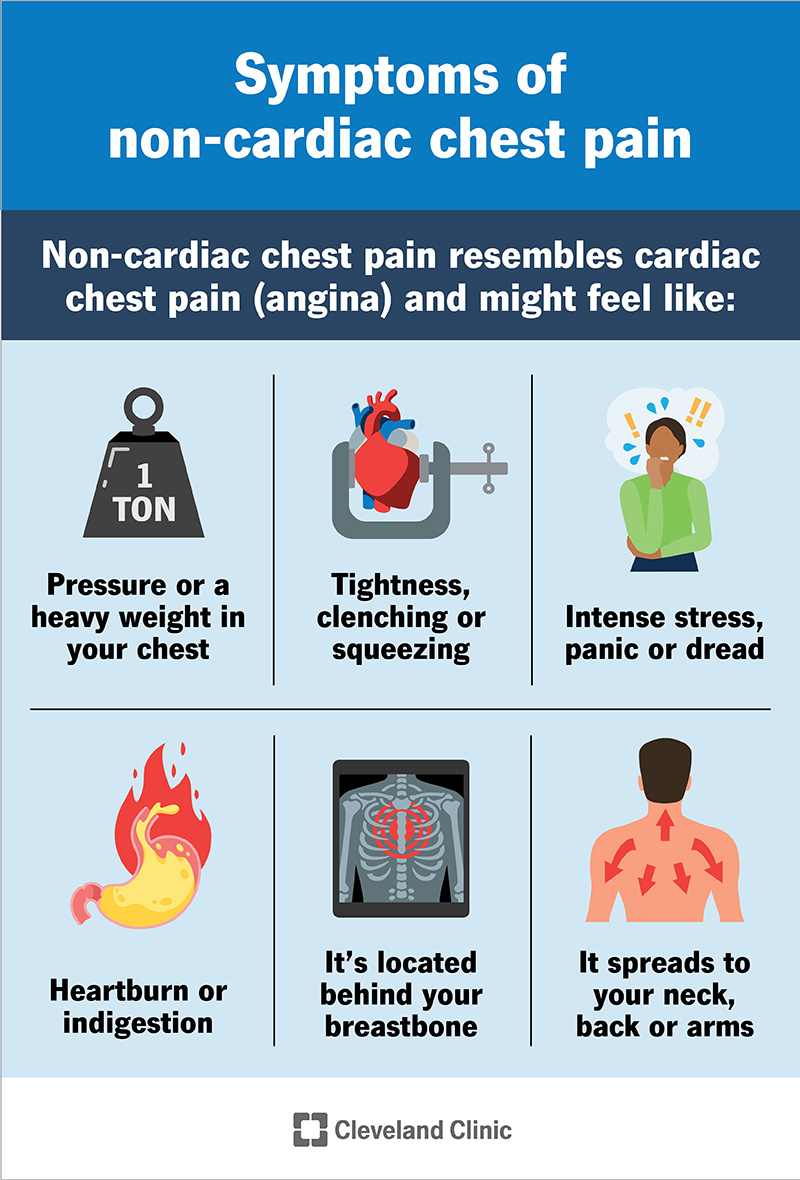
Noncardiac chest pain resembles cardiac chest pain (angina). It might feel like:
Like cardiac chest pain, noncardiac chest pain may start after a stressful event or after a large meal. It may last from a few seconds to a few hours. If it lasts longer than a few minutes, you should seek care.
Unlike cardiac chest pain, noncardiac chest pain is unlikely to:
Advertisement
GERD (chronic acid reflux) is the most common cause of noncardiac chest pain, and of chest pain in general. When gastric acid escapes from your stomach and backwashes into your esophagus, it burns it on the inside, causing pain. You feel it in your chest because your esophagus runs through your chest.
Other possible causes include:
You may be more likely to experience noncardiac chest pain if you:
Doctors diagnose noncardiac chest pain after ruling out cardiac causes. If you experience symptoms that resemble cardiac chest pain, you should go to the emergency room. A healthcare provider will review your symptoms, take your vital signs and screen you for a heart attack or heart disease.
Common screening tests include:
After ruling out cardiac conditions, they’ll diagnose noncardiac chest pain. They might refer you to a gastroenterologist next. Gastroenterologists can diagnose and treat conditions related to your esophagus. They can screen you for GERD and other esophageal disorders, as well as digestive diseases.
These tests might include:
Sometimes, a healthcare provider might try treating you with medications for GERD before testing for it. This is just a different way of screening you for GERD. If proton pump inhibitors (PPIs) relieve your chest pain, your provider can confidently diagnose GERD chest pain. If not, they can proceed with further tests.
Advertisement
Treatment for noncardiac chest pain depends on the causes. Common treatments include:
Treating noncardiac chest pain may be simple or complex, depending on the cause. Most people respond to proton pump inhibitors or antidepressant pain modulators. If you have a more complex condition, you might need more extensive treatment, or a combination of different approaches.
Noncardiac chest pain isn’t generally life-threatening, but it can affect your quality of life. Anything that feels like cardiac chest pain can be scary and stressful to experience. And sometimes, the condition causing it can damage your body over time. Any recurring pain deserves care, especially chest pain.
Advertisement
Cleveland Clinic’s primary care providers offer lifelong medical care. From sinus infections and high blood pressure to preventive screening, we’re here for you.

Last reviewed on 07/02/2025.
Learn more about the Health Library and our editorial process.