Double inlet left ventricle is a congenital heart problem in which the atria of your baby’s heart both supply blood to the left ventricle. Treatment includes open-heart surgeries to correct the blood flow to your baby’s lungs and body. The survival rate is fairly good. Many babies live to adulthood due to advances in surgical procedures.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
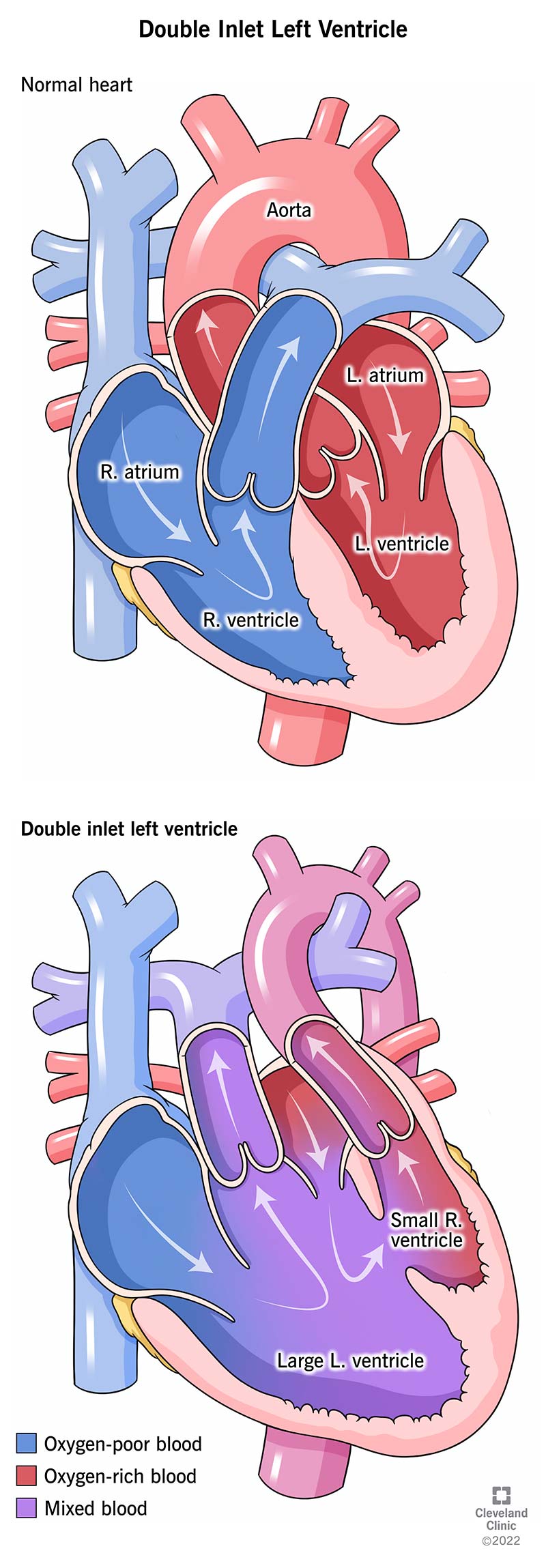
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/14786-double-inlet-left-ventricle)
Double inlet left ventricle is a rare congenital heart defect, meaning it’s present at birth. With this condition, your baby’s heart has only one functioning lower heart chamber — the left ventricle. The upper chambers of your baby’s heart — the left and right atria (plural for atrium) — are both connected to the left ventricle. Double inlet left ventricle is a type of single ventricle defect.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The human heart has four sections (chambers): the left atrium and right atrium at the top and the left and right ventricles at the bottom. Blood circulates through the atria and ventricles. The atria receive blood from the veins, and the ventricles pump blood out through the arteries.
In a normal heart, the right atrium receives blood that needs oxygen from large veins called vena cava. The blood enters the right ventricle, which pumps blood to the lungs via the pulmonary arteries to pick up oxygen. The blood returns to the heart at the left atrium, where it’s collected and passed into the left ventricle. The left ventricle then pumps this oxygenated blood through a large artery called the aorta to the rest of the body.
Babies born with a double inlet left ventricle usually have a functioning left ventricle and a small right ventricle. The right ventricle usually has limited function. Both atria supply blood to the left ventricle. As a result, oxygen-rich blood and oxygen-poor blood mix together in your baby’s heart. The mixed blood flows to your baby’s lungs and body.
Double inlet left ventricle is very rare. The condition occurs in 0.05 to 0.1 of every 1,000 live births. It accounts for about 1% of all congenital heart issues.
Advertisement
Double inlet left ventricle symptoms usually appear very early in a baby’s life, from a few days to a few weeks of life. These symptoms may include:
The cause of double inlet left ventricle is unknown, but the defect likely occurs early during pregnancy while your baby’s heart is developing.
Many babies with double inlet left ventricle have other abnormalities in their heart or their main arteries. These abnormalities can block blood flow to their lungs. These may include:
During pregnancy, a healthcare provider may perform a fetal echocardiogram test to listen to the fetus’s heart. You may get this test between weeks 18 and 24 of your pregnancy. It uses sound waves (ultrasound) to create an image of the fetus’s heart. Your provider may recommend a fetal echocardiogram if:
After your baby is born, their healthcare provider will test them for heart problems as part of their newborn screening. Newborn screening includes blood, hearing and heart checks. Your baby’s provider will screen them for heart conditions using pulse oximetry (pulse ox). This test checks your baby’s blood oxygen level. Low levels of oxygen can signal a problem with the heart.
Your baby’s healthcare provider will also perform a physical examination. They’ll listen to your baby’s heartbeat and check their vital signs.
Your baby’s healthcare provider may order various tests to diagnose or confirm your baby’s condition. These tests may include:
Advertisement
Double inlet left ventricle treatment includes surgery to balance and optimize blood flow to your baby’s lungs and body. Your baby may need several surgeries to make their heart work effectively. These are open-heart surgeries and may include:
Your baby’s surgeon will perform the first surgery within the first few days to weeks of your baby’s life. They’ll use a small tube called a shunt to direct blood flow to your baby’s lungs. A pediatric cardiologist will decide when your baby should have the second surgery.
Your baby’s surgeon will perform the second surgery when your baby is 4 to 6 months old. They’ll direct the blood flow from your baby’s upper body to their pulmonary artery so blood can collect oxygen from your baby’s lungs without going through their heart.
Your child’s surgeon will perform the final procedure when your child is 2 to 3 years old. They’ll separate the circulation, so no mixing of your child’s blood occurs. After this final stage of surgery, your child’s oxygen levels will be similar to a child with a normal heart. Although the Fontan procedure doesn’t result in normal blood circulation in your child’s body, it improves circulation and allows your child to grow.
Advertisement
Your child’s healthcare provider may prescribe certain medications before and after the surgeries. These medications may include:
In addition, your child will have to take antibiotics before any dental treatments to prevent endocarditis (infection of the heart lining).
In the most severe cases of double inlet left ventricle, your baby’s healthcare provider may recommend a heart transplant.
The 10-year survival rate of babies with double inlet left ventricle is between 70% and 80%. Many babies with the condition live to adulthood due to advances in surgical procedures. Factors that affect your baby’s double inlet left ventricle prognosis include:
Children with double inlet left ventricle need regular follow-ups. In addition, they may face various complications, and their physical activity may be limited. Complications of double inlet left ventricle may include:
Advertisement
You can’t prevent double inlet left ventricle because the condition’s cause isn’t known. However, you can take steps to ensure a healthy pregnancy before you’re even pregnant. Ways to take care of yourself include:
The last thing an expectant parent wants to hear is there’s something wrong with the fetus. You can’t prevent double inlet left ventricle, but you can take steps during your pregnancy to reduce the likelihood of environmental effects. It’s normal to feel concerned, anxious or scared when learning about your baby’s congenital heart condition. Discuss your concerns with your healthcare provider. They can help you better understand the condition and what to expect.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Whether you were diagnosed as a child or later in life, Cleveland Clinic is here to treat your adult congenital heart disease.
