Mediastinal tumors include thymomas, lymphomas, germ cell tumors and cysts, among others. They’re masses of cells that appear in the space between your lungs, called the mediastinum. These tumors may be malignant (cancerous), but they’re usually benign (noncancerous). Surgery is the most common treatment.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
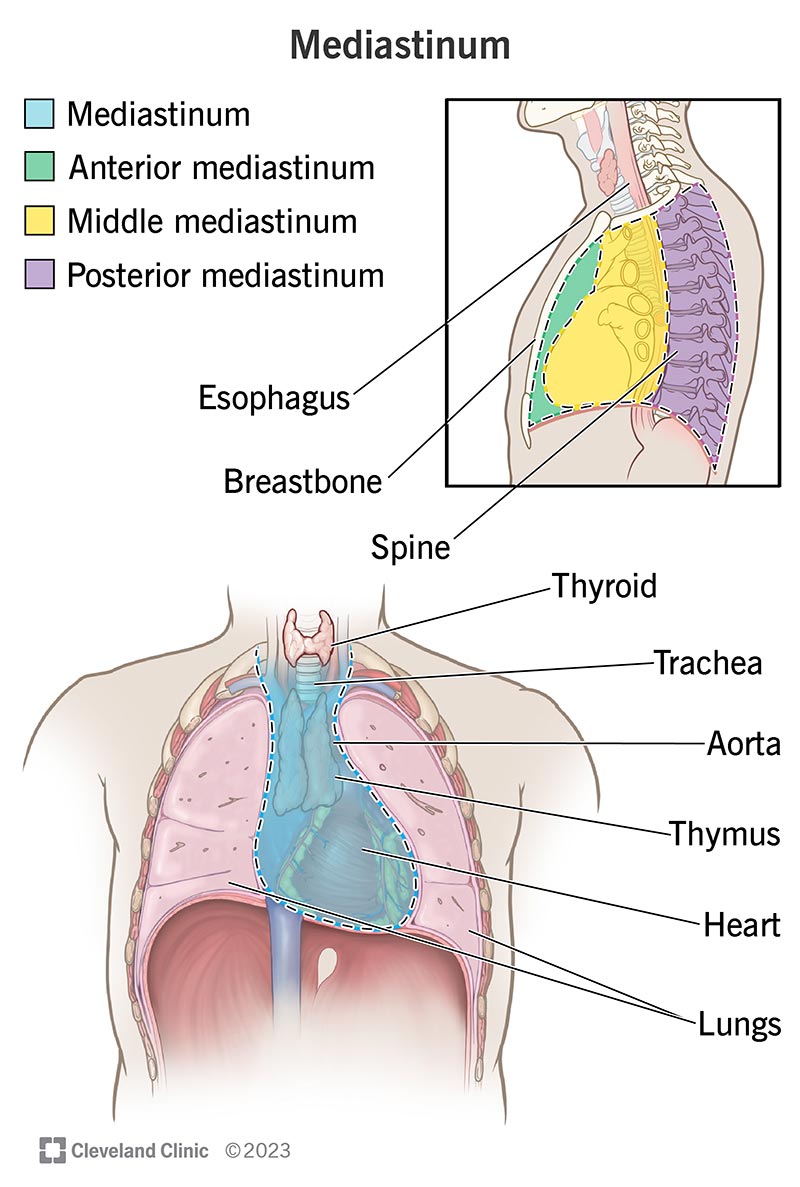
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/13792-mediastinal-tumors)
Tumors (also called neoplasms) are masses of cells. They can be benign (not cancerous) or malignant (cancerous). Mediastinal tumors are growths that form in the area of your chest between your lungs.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
This area, called the mediastinum, is surrounded by your breastbone in front, your spine in back and your lungs on each side. Your mediastinum contains your heart, aorta, esophagus, thymus, thyroid, trachea, lymph nodes and nerves. Your thymus is an organ that’s part of your immune system. Your lymph system, or lymphatic system, is also part of your immune system and helps protect your body.
There are several types of mediastinal tumors. They’re classified based on where they are in your mediastinum: the anterior (front), middle or posterior (back).
Advertisement
Most people diagnosed with mediastinal tumors are between the ages of 30 and 50. Still, these tumors can develop at any age and form from any tissue that exists in or passes through your chest cavity.
In adults, most tumors form in the anterior (front) mediastinum and are cancerous lymphomas or thymomas.
In children, most tumors form in the posterior (back) mediastinum. These tumors often begin in the nerves and aren’t cancerous.
Mediastinal tumors are rare, occurring in less than 1% of the population. Most form in the anterior (front) part of your mediastinum. The most common types are thymomas, benign mediastinal cysts and lymphomas.
Due to their location, mediastinal tumors that aren’t treated can cause serious problems, even if they’re not cancerous. These issues include spreading to your heart, pericardium (the lining around your heart) and great vessels (the aorta and vena cava). Tumors in your posterior (back) mediastinum can place pressure on your spinal cord.
Only about 25% of mediastinal masses are cancer. However, the chance of a malignant tumor increases if it’s in the front part of your mediastinum. Approximately 60% of anterior mediastinal masses are cancerous.
Almost 40% of people with mediastinal tumors don’t notice symptoms. Instead, healthcare providers often discover these tumors incidentally during chest X-rays performed for other reasons.
Advertisement
Symptoms often result from the tumor putting pressure on surrounding structures, like your heart, airway or spinal cord. Generally, children experience symptoms more commonly than adults. Malignant tumors cause symptoms more often than benign tumors.
Symptoms of a mediastinal tumor may include:
Mediastinal tumors form for different reasons, including:
Advertisement
When a mediastinal mass, or tumor, appears on a chest X-ray, healthcare providers often perform additional tests, like imaging or bloodwork, to learn more about it. Your healthcare provider may also perform tests if you have symptoms and a medical history that suggests a mediastinal mass.
The tests most commonly used to diagnose and evaluate a mediastinal tumor include:
Advertisement
Treatment for mediastinal tumors depends on the type of tumor, its location, its stage (if it’s cancerous) and your symptoms. Surgery is the most common treatment.
Every type of tumor is different. The outlook varies based on the type of tumor, whether the tumor’s cancerous and your general health.
Ask your healthcare provider about likely treatment outcomes. If you have a cancerous tumor, like a thymoma or lymphoma, ask your healthcare provider about cure rates and survival rates based on your unique diagnosis.
Mediastinal masses aren’t preventable. But you can improve your chance of successful treatment if a healthcare provider finds your tumor early. See a healthcare provider if you have shortness of breath, coughing or other symptoms lasting longer than two weeks.
Questions to ask include:
Various tumors can form in your mediastinum. Some are serious and require immediate treatment. With others, you may not experience symptoms or need treatment at all. Your healthcare provider can explain your tumor type and whether it’s serious. Often, your provider can remove tumors causing symptoms with minimally invasive procedures like video-assisted thoracic surgery (VATS). Ask your healthcare provider about likely outcomes based on the type of tumor you have.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
When you’re diagnosed with cancer, you want expert and compassionate care right away. At Cleveland Clinic we personalize your treatment to match your needs.
