Kawasaki disease is a rare condition characterized by fever and inflamed blood vessels in children under 5. Researchers don’t know the cause, but they’ve found treatments that work for many. Prompt treatment is important for a good prognosis. The risk is greatest when Kawasaki disease affects the arteries that supply blood to your child’s heart.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Kawasaki disease or Kawasaki syndrome is a rare type of vasculitis (blood vessel inflammation). Inflamed blood vessels can become weak and stretched out. When that happens, they’re at risk of tearing. They can also develop scarring and become too narrow. This limits how much blood can get through to nourish tissues and organs.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Kawasaki disease happens most often in children 6 months to 5 years of age. It affects all of their arteries, but the biggest concern is their coronary arteries. These supply blood to their heart. Children with affected coronary arteries can have heart issues as a result.
With prompt treatment, most children recover in about two months.
Kawasaki disease is rare, occurring in an estimated 10 to 20 out of 100,000 children younger than 5 in the United States and Canada. In Japan, Korea and Taiwan, it affects 50 to 250 out of 100,000 children younger than 5.
Kawasaki disease is the most common cause of acquired heart disease in children in the United States, Japan and other developed countries.
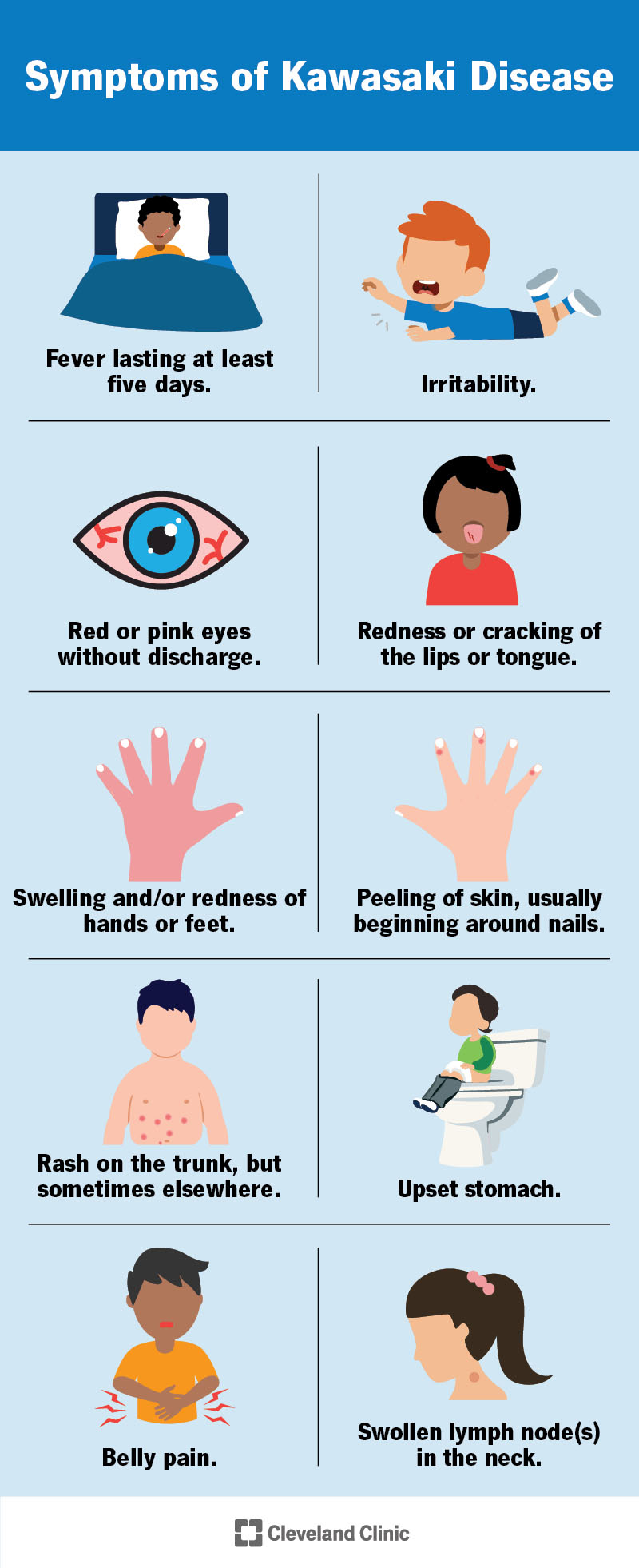
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/13457-kawasaki-disease-illustration)
Kawasaki disease symptoms can include:
The cause of Kawasaki disease is unknown, although more cases happen in late winter and early spring. Researchers are looking into possible Kawasaki disease causes like infections, environmental factors or genetics.
Advertisement
No. Even though a rash is one of the symptoms, it doesn't spread through person-to-person contact.
Risk factors for Kawasaki disease include:
You can still get Kawasaki disease even if you don’t have any of these risk factors.
Complications of Kawasaki disease include:
Symptoms and signs help healthcare providers make a Kawasaki disease diagnosis with a physical exam. If your child only has some of the symptoms, this is atypical or incomplete Kawasaki disease. Before making a diagnosis, providers have to rule out other causes of fever.
The three stages of Kawasaki disease are:
Stage 1 (Acute)
Stage 2 (Subacute)
Stage 3 (Convalescent)
There’s no test that can directly detect Kawasaki disease. But healthcare providers can do tests that support a diagnosis of Kawasaki disease or rule out other possible illnesses.
They may order:
Treatment for Kawasaki disease includes:
Advertisement
Your child will be in the hospital for treatment. The goals of Kawasaki disease treatment are to:
IVIG is usually well tolerated, but can cause:
Anticoagulants can make your child bleed more easily.
The reasons for admission vary, but evaluation for Kawasaki disease usually takes place in the hospital.
Your child will be ready to go home from the hospital when they’re:
You’ll need to follow up with your primary healthcare provider, an infectious disease doctor and a cardiologist after discharge. They’ll follow your child closely, including repeating lab work, until there’s no longer any need for further therapy.
A cardiologist will order follow-up echocardiograms one to two weeks and four to six weeks after hospital discharge. Your child may need more frequent echocardiograms if they had issues with their coronary arteries.
Advertisement
Children can have Kawasaki disease symptoms for four to six weeks. They may feel tired and irritable for eight weeks.
Kawasaki disease can come back in about 2% or 3% of cases.
It can cause long-term damage to arteries and possible heart issues in adulthood. Atherosclerosis is one example. People who have aneurysms (dilated coronary arteries) from the disease need long-term follow-up every year or a few years for the rest of their lives. In some cases, they may need a procedure to improve blood flow.
Your child’s provider will want to make sure they don’t develop blood clots. They also want to make sure your child’s heart muscle gets enough oxygen.
The outlook for children with Kawasaki disease depends on how much it affects their hearts. Complications that affect their heart can be severe enough to be fatal within 15 to 45 days of a fever starting. Fortunately, treatment can usually keep heart disease from occurring.
Coronary artery aneurysms can happen in 25% of people who don’t get treatment. In children who receive timely treatment, the rate of coronary artery aneurysms is less than 6%. With treatment, 50% of children with affected coronary arteries heal in one to two years.
Yes. But with prompt treatment, most children with Kawasaki disease can recover completely.
Advertisement
No. Because researchers don’t know what causes Kawasaki disease, they don’t know how to prevent it.
You can care for your child by:
Contact your healthcare provider if your child has:
Questions to ask your provider include:
It’s not easy to see your child experiencing a fever and other symptoms. But researchers have found treatments that have helped many children over the years. Ask your child’s healthcare provider if you can bring a favorite toy or blanket to the hospital to soothe your child. Your touch and calming voice can help them feel more at ease while dealing with symptoms.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When your child has a serious condition like Kawasaki disease, you want help right away. Cleveland Clinic Children’s experts can provide treatment quickly.
