Arachnoiditis is a rare pain disorder caused by inflammation of the arachnoid, one of the membranes that surrounds the nerves of your spinal cord. It can cause severe pain and neurological symptoms, such as muscle weakness. Arachnoiditis has several possible causes, and treatment is aimed at managing symptoms.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
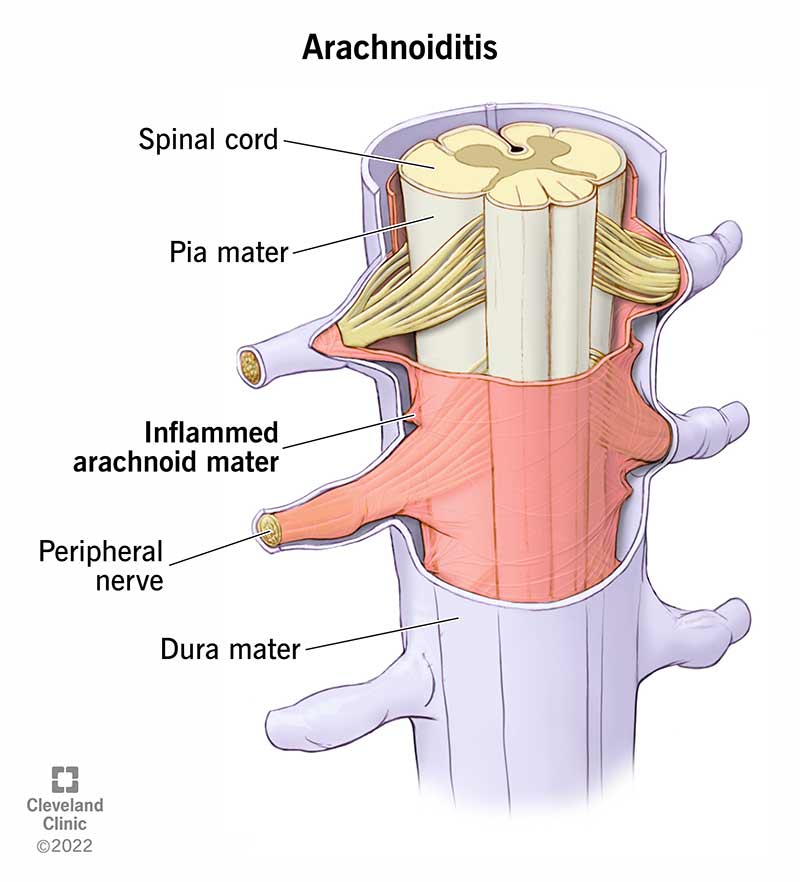
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/12062-arachnoiditis)
Arachnoiditis is a rare pain disorder caused by inflammation (swelling) of the arachnoid, one of the membranes that surrounds and protects the nerves of your spinal cord.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Arachnoiditis causes severe stinging, “burning” pain and neurological problems. It most commonly affects the nerves of your lumbar (low back) and thoracic spine (middle back). It rarely affects your entire spine.
The course of this condition remains highly variable since arachnoiditis can be either a static (stays the same) or progressive (gets worse over time) disease.
The arachnoid mater is part of the meninges, which are three layers of membranes that cover and protect your brain and spinal cord (your central nervous system). The arachnoid mater is the middle layer. The other two layers are the dura mater and pia mater.
There are three spaces within the meninges:
Advertisement
Arachnoiditis affects the arachnoid layer somewhere along your spinal cord, not your brain.
In arachnoiditis, damage to and inflammation of the arachnoid (subarachnoid or subdural space) leads to a cascade of events, including:
Due to these changes in the arachnoid and nerve roots, arachnoiditis frequently results in pain and possible neurological deficits, such as muscle weakness and sensory issues.
As arachnoiditis progresses, it can lead to the formation of scar tissue and cause the spinal nerves to stick together and malfunction (not work properly). This leads to a condition called chronic adhesive arachnoiditis.
Adhesive arachnoiditis can potentially lead to disability. Many people with the condition eventually need to use a wheelchair due to paraparesis, which occurs when you're partially unable to move your legs.
Arachnoiditis is rare, but researchers don’t know exactly how widespread it is. Since the presentation of arachnoiditis ranges from very mild to severe, many mild cases of arachnoiditis will either never be diagnosed or aren’t reported.
Recent studies show that the frequency of lumbar arachnoiditis appears to be increasing due to an increasing amount of lumbar spine surgeries.
While it’s not life-threatening, the chronic pain and neurological issues associated with arachnoiditis can greatly affect your quality of life. It’s important to find a healthcare provider who’s familiar with arachnoiditis to receive the best treatment.
Arachnoiditis has no consistent pattern of symptoms, though the most common symptom is pain. The symptoms can vary based on which part of your spine (which spinal nerve) is affected and can range from mild to severe.
Arachnoiditis most commonly affects the nerves connecting to your lower back and legs (lumbar spine).
Arachnoiditis can cause many symptoms, including:
Advertisement
Symptoms may become more severe or even permanent if the condition progresses. Many people with arachnoiditis are unable to work and have a significant disability because of constant pain.
In many cases of arachnoiditis, healthcare providers aren’t able to determine the exact cause. This is because it’s a rare condition with multiple possible causes, and the symptoms can appear a while after the incident that caused it.
The arachnoid can become inflamed because of irritation from one of the following sources:
Advertisement
Less commonly reported causes of arachnoiditis include:
Arachnoiditis can be difficult to diagnose since it’s rare and not all healthcare providers are familiar with it. There are also no reliable laboratory tests or imaging test findings to definitively diagnose arachnoiditis. Providers base the diagnosis on clinical presentation and symptoms, along with supporting MRI or CT myelography.
If you have symptoms of arachnoiditis, your healthcare provider may order the following tests to help diagnose it:
Advertisement
Unfortunately, there’s no cure for arachnoiditis. Treatment mainly focuses on alleviating pain, improving quality of life and managing symptoms.
Treatment options for arachnoiditis are similar to those for other chronic pain conditions. Often, healthcare professionals recommend a program of the following:
Specific types of treatment include:
Arachnoiditis is usually chronic (lifelong) and may be progressive, meaning it gets worse over time. While there are therapies and treatments that can help manage symptoms, there’s no cure.
The quality of life of people with severe arachnoiditis is often poor due to significant neurological symptoms and pain.
Arachnoiditis may cause disability in some people, and they may be unable to work full time due to constant pain and various neurological issues. Many people with arachnoiditis, however, can walk and drive a car without significant limitations.
Unfortunately, there’s no known way to prevent arachnoiditis.
Besides following your healthcare provider’s plan for managing your symptoms, such as medications and therapy, it’s important to take care of yourself. The following actions can help you cope with chronic pain and improve your overall health:
If you have chronic pain and depression and/or anxiety, it’s important to seek treatment for your mental health condition(s) as well. Having depression or anxiety can make your chronic pain worse. For example, if you have depression, the fatigue, sleep changes and decreased activity may worsen your chronic pain.
If you’ve been diagnosed with arachnoiditis, you’ll need to see your healthcare provider regularly to monitor your symptoms and treatment plan.
It’s never easy to live with chronic pain. Since arachnoiditis can affect both your physical and mental health, it’s essential to seek proper treatment and advocate for yourself. Joining a support group — whether online or in-person — or finding other healthy, therapeutic outlets to manage your stress can help lighten the load. Be sure to seek out a healthcare provider who’s familiar with arachnoiditis. They can help determine the best treatment plan for you to manage your symptoms.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Comprehensive pain recovery treatment plans can help you manage your pain levels and symptoms more easily.
