A spinal cord stimulator (SCS) is a medical device that treats chronic pain. Your provider may suggest an SCS if you have pain that hasn’t responded to other forms of treatment. You’ll need two surgeries. One for a trial phase, and then a second to permanently implant the device.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
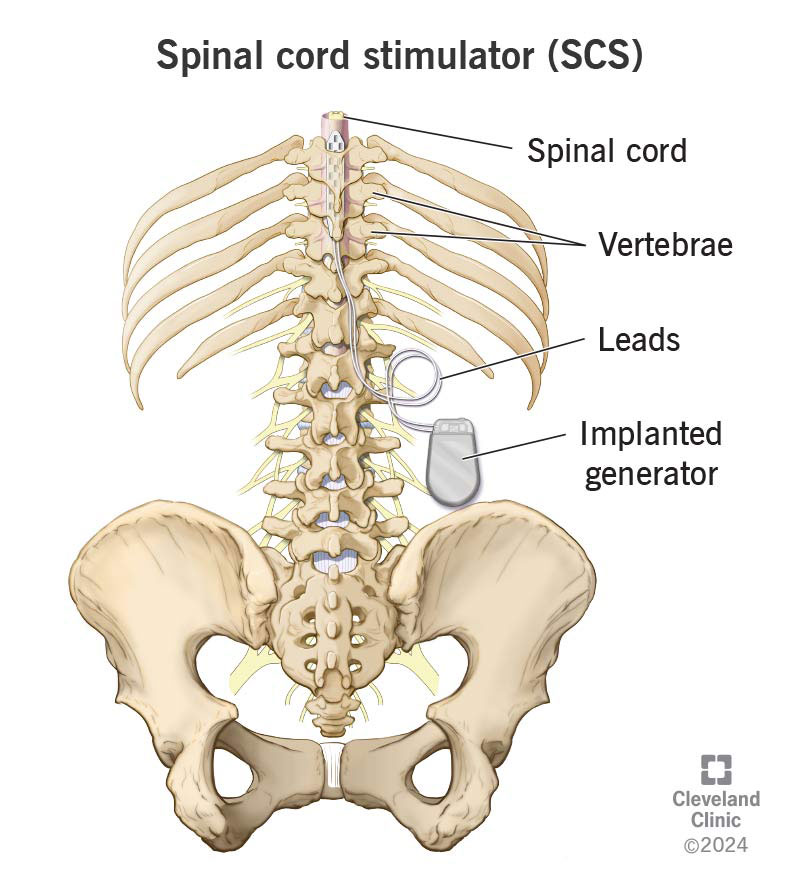
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/spinal-cord-stimulator)
A spinal cord stimulator (SCS) is a medical device that a surgeon implants in your body to help treat severe pain.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your healthcare provider will usually suggest other, nonsurgical treatments, like physical therapy and medications, before a spinal cord stimulator. But an SCS may be a good option if other treatments haven’t worked or it’s not safe for you to take certain medications, like opioids.
A spinal cord stimulator works by toning down chronic pain signals in your body. Pain signals are electrical currents that start in your nerves, travel along your spinal cord and up to your brain. Your brain translates these electrical signals into the pain you feel. An SCS emits a safe, alternate electrical current into your spinal cord that you can control. This other current can block the chronic pain signals and help your brain ignore them.
A spinal cord stimulator is like a really good white noise machine. The hum of a sound you choose to turn on in a room can block out annoying noises you don’t want to hear. It doesn’t eliminate the problem (the pain signals), but it helps you and your brain tune them out so you can focus on working, sleeping and all of your other daily activities.
You’ll use a remote to control the SCS when you’re feeling pain. You’ll be able to adjust to respond to different types and levels of pain.
Advertisement
Lots of health conditions and injuries can cause chronic pain. Your provider may recommend a spinal cord stimulator to manage:
These are just some examples. Researchers are still studying how spinal cord stimulators can help people manage other types of pain. Your provider will tell you if an SCS is a good option for you.
Your surgeon will tell you what you need to do to get ready for surgery. In general, you’ll need:
Tell your provider and surgeon which medications and over-the-counter supplements you take. You may have to stop taking some medications or supplements before surgery.
Getting a spinal cord stimulator is a two-step process. First, you’ll have a trial period. Your surgeon will put a temporary version of the SCS into your body. It’s a non-permanent option that lets you try spinal cord stimulation before they permanently insert one.
You’ll be able to get a sense for how the spinal cord stimulator works, and if it’s right for you. Your surgeon will probably suggest that you try the temporary SCS for a few weeks before deciding if you want the permanent version.
If the trial SCS manages the pain and you feel comfortable with using the device, your surgeon will implant the permanent spinal cord stimulator. A successful trial usually means the SCS reduces the pain you feel by at least half.
The steps for a spinal cord stimulator trial and the permanent implant are slightly different. For both surgeries, an anesthesiologist will give you anesthesia to numb your spine and back so you don’t feel pain during the surgeries. You might need general anesthesia that puts you to sleep.
Your surgeon will implant a temporary spinal cord stimulator into your back for your trial. Your surgeon will:
Advertisement
You’ll wear the external generator throughout the trial phase. When you feel pain, you can use the remote to control the current to the SCS. Your surgeon will show you how to control the stimulator.
If you’re happy with how well the trial spinal cord stimulator manages pain, your surgeon will implant a permanent version a few weeks later.
The steps for a permanent SCS implant are similar to the trial. Your surgeon will:
Advertisement
The surgery for an SCS trial is usually outpatient. This means you can go home the same day.
Your surgery care team will tell you how to take care of the incisions after both surgeries. You’ll need to keep your surgery sites clean and change the bandages on them for around a week. They’ll also make sure you know how to use the SCS remote and adjust it before you go home.
You’ll have a follow-up appointment about two weeks after the permanent implantation surgery. A provider will remove the staples and/or stitches around the generator.
A spinal cord stimulator is a safe, effective way to manage pain that other treatments haven’t.
An SCS can help you manage pain with less medication. It can help prevent side effects from pain medications, especially if you can’t take opioids. You may be able to reduce how much pain medication you take. You may end up not needing any at all.
The trial phase is also a benefit. There aren’t many surgeries that let you test drive them to see if they’ll work for you. You can try an SCS without having to commit to permanent surgery right away. If the trial doesn’t work as well as you’d hoped, you don’t have to get the permanent implant.
All surgeries have risks. Some complications that can happen from both kinds of SCS surgery include:
Advertisement
Some people worry about their body rejecting the implanted leads or generator. These devices aren’t like an organ transplant that can experience rejection when your body’s immune system attacks it. Talk to your surgeon or healthcare provider if you’re feeling any new or changing pain around your implants.
You’ll need to take it easy and rest after both the trial and permanent implant surgeries. You’ll probably need to avoid some movement and motions, including:
You won’t be able to get the leads or external generator wet during the trial phase. Avoid swimming, hot tubs and baths. You might need to keep yourself clean without getting in the shower. Your surgeon will tell you if it’s safe.
Your surgeon will also tell you when it’s safe to resume your usual routine. You’ll need four to six weeks after the permanent implant surgery to get used to the stimulator leads and their effects. This gives your body time to heal around the implanted generator and leads.
The batteries in a permanent SCS implant last a long time. Most will last for at least 10 years. Some models are rechargeable. If yours is, you’ll hold a charger near your skin to recharge the battery. Your surgeon will show you how to do this.
You should be able to resume many of your usual activities once your body heals around the implants. Many people can get back to activities that pain made them avoid in the past. But there are some things to keep in mind:
A spinal cord stimulator’s success rate can vary. It depends on which condition you’re using it to manage and how severe the pain is to begin with. Most people experience half as much pain.
Sometimes, spinal cord stimulators can lose effectiveness over time for unknown reasons. Talk to your surgeon. They’ll give you a better idea of what you can expect based on your unique circumstances.
Your surgeon will schedule follow-up visits after the permanent implant surgery. They’ll help you adjust to the electrical stimulation from your SCS.
Go to the emergency room if you notice any severe side effects, including:
Most of the time, pain is your body’s way of telling you something is wrong or hurting you. It’s like a built-in alarm system that tells you to pay attention to a part of your body.
But chronic pain overstays its welcome. It’s more than a heads-up that you need to focus on an issue. It’s severe pain that can make it hard to sleep or work. It can be exhausting. Especially if it feels like you’ve tried every other treatment and nothing’s worked. A spinal cord stimulator (SCS) might sound intimidating at first. But it can be a great option if other treatments haven’t helped you feel like yourself.
Unlike a lot of surgical procedures, you’ll get a trial period to see how an SCS can help manage the pain you feel. It’s a safe, effective surgery, but don’t be afraid to ask a lot of questions at any point. Your surgeon will help you understand everything you need to know to make the best decision to manage that pain.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
The neurosurgery care team at Cleveland Clinic helps find solutions for your brain, spine and nerves — whether that means surgery or not.
