Neurologists use electromyography (EMG) to help diagnose injuries and conditions that affect your muscles and the nerves that control them, such as carpal tunnel syndrome and muscular dystrophy. They often use this test alongside a nerve conduction study.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
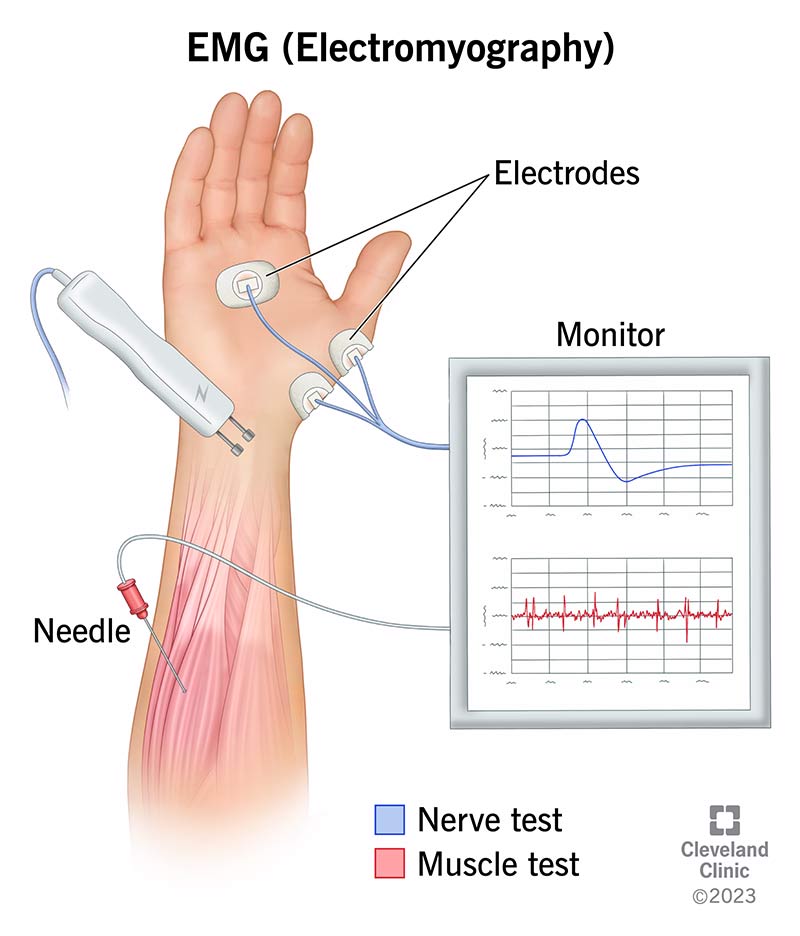
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/4825-electromyography)
Electromyography (EMG) is a diagnostic test that evaluates the health and function of your skeletal muscles and the nerves that control them. It’s one form of electrodiagnostic testing.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Every body movement you make, from lifting your leg to nodding your head, involves complex communication between your central nervous system (your brain and spinal cord), nerves and muscles. To produce movement, your motor (movement) nerves send electrical signals to your muscles. An EMG can detect issues with your motor nerves, muscles or the communication between the two.
Neurologists often perform an EMG test alongside a nerve conduction study (NCS). An NCS measures the flow of electrical current through a nerve before it reaches a muscle. An EMG measures the response of muscles to electrical activity and how much electrical activity a muscle contraction produces.
Your healthcare provider may recommend an EMG if you have symptoms such as muscle weakness or numbness and tingling. You may have an EMG in an outpatient setting or as part of your stay in a hospital, depending on your situation.
An EMG can help diagnose several injuries or diseases that affect your motor nerves and muscles. It can help determine the presence, location and extent of these injuries and diseases. Providers may also use EMG tests to rule out conditions.
Categories of conditions an EMG can help diagnose include:
Advertisement
Providers use other tests in conjunction with electromyography to diagnose these conditions, such as imaging tests, blood tests and muscle biopsies.
To understand how an EMG test works, it helps to understand how your muscles work.
Your motor nerves (motor neurons) send electrical signals to your muscles to tell them what to do. (These signals originate in your brain, travel down your spinal cord, through your motor nerves and to your muscles.) This electrical stimulation causes electrical activity in your muscles, which causes them to contract (tighten). The muscle contraction itself also produces electrical activity.
Normally, a muscle at rest has no electrical activity. A slight contraction of the muscle results in some electrical activity, which increases as the muscle contracts more intensely.
In electromyography, a healthcare provider inserts a small needle with an electrode into one of your muscles to record its electrical activity. The provider doesn’t deliver electrical stimulation through the needle. Instead, you can think of the needle as being similar to a microphone — it’s only a recording device.
As you rest or contract your muscle, the needle electrode records the electrical activity. The needle is attached through a cable to a computer that allows the provider to see what your muscle is doing both at rest and with movement. It appears as waves on a screen. They may also use an audio amplifier so they can hear the pulses of electrical activity.
The provider then analyzes these readings to look for signs of issues. For example, if your muscle is damaged, it may have abnormal electrical activity when it’s resting. When it contracts, its electrical activity may make abnormal wave patterns.
Before you have an EMG, you should:
Advertisement
In some cases, your provider may instruct you to not smoke cigarettes or drink caffeinated beverages, such as coffee or tea, two to three hours before testing. These substances may interfere with the test.
Neurologists usually perform an EMG test right after a nerve conduction study. During the nerve conduction study, a provider will put electrodes (stickers) on the surface of your skin. They’ll then deliver a small electrical impulse that will feel like a shock to nerves and record the response. In most cases, they’ll test several different nerves.
The process can vary for an EMG, depending on the reason for the test and which muscles and nerves the provider is assessing. But in general, you can expect the following during an EMG test:
Advertisement
You may feel some pain or discomfort when your provider inserts the needle into your skin and muscles. But most people can complete the test without issues.
After the test, the muscles they tested may feel tender for a few days.
The test usually takes 60 to 90 minutes. It depends on how many muscles your provider needs to test.
You may have sore or tender muscles for a few days after the test. The muscle soreness isn’t usually severe and should get better in less than a week. You may also see some bruising where the needles entered your skin.
EMG is generally safe. Complications are rare. Some people (especially people who take blood thinner medications) may bleed after the test.
Although EMG tests can be very helpful, they alone don’t usually provide a diagnosis. Your healthcare team providers will assess the results in conjunction with other medical tests to determine a diagnosis.
You can expect to receive the results of the test typically within 24 to 48 hours after the testing is completed.
Call your healthcare provider if you have:
Advertisement
An EMG can help diagnose a pinched nerve and issues related to it, but it can’t “show” a pinched nerve. Imaging tests like X-rays, CT scans and MRI scans help healthcare providers see a pinched nerve and what’s causing it (such as a herniated disk).
If you have signs of muscle disease, nerve damage or injury, an electromyography (EMG) test will help your provider learn more about what’s going on. It also helps your provider plan treatment. If you have any questions about the test, don’t hesitate to ask. Your provider is available to help and support you.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
If you have a neurological condition, you want expert advice. At Cleveland Clinic, we’ll work to create a treatment plan that’s right for you.
