Menopause is a point in time when a person has gone 12 consecutive months without a menstrual period. Menopause is a natural part of aging and marks the end of your reproductive years. On average, menopause happens at age 52.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_26b79p4b/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Lynn Pattimakiel, MD, explains the common symptoms associated with menopause and the importance of monitoring them.
Menopause is a point in time when you’ve gone 12 consecutive months without a menstrual period. It happens, on average, at age 52. It’s a natural process that occurs when your ovaries stop producing reproductive hormones. When menopause happens due to surgery or medical treatment, it’s called induced menopause.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Hormonal changes due to menopause can cause uncomfortable physical and emotional symptoms. There are treatments available to help with symptoms of menopause, like hormone therapy, medication or lifestyle adjustments.
Menopause is the permanent ending of menstruation. If it doesn’t happen because of any type of medical treatment or surgery, the process is gradual and happens in three stages:
Advertisement
Menopause, when it occurs between the ages of 45 and 55, is considered “natural” and is a normal part of aging. Menopause that occurs before the age of 45 is called early menopause. Menopause that occurs at 40 or younger is considered premature menopause. When there’s no medical or surgical cause for premature menopause, it’s called primary ovarian insufficiency.
The average age of menopause in the United States is 52 years old. But the transition to menopause usually begins in your mid-40s.
Menopause is a point in time, so you don’t stay in menopause. You reach it when you haven’t gotten a menstrual period for one year. Immediately after you reach menopause, you move into postmenopause. This stage lasts for the rest of your life.
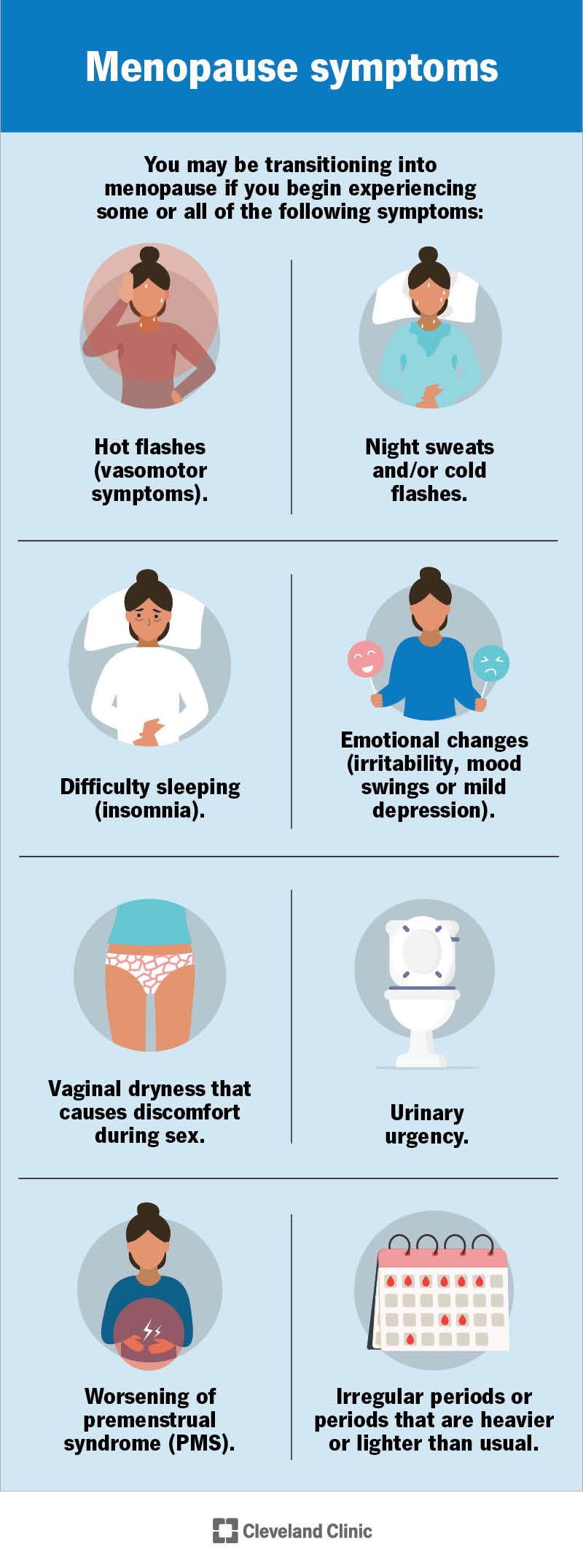
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/21841-menopause)
You may be transitioning into menopause if you begin experiencing some or all of the following symptoms:
Some people might also experience:
Changes in your hormone levels cause these symptoms. Some people have intense symptoms of menopause, while others have mild symptoms. Not everyone will have the same symptoms as they transition to menopause.
Contact a healthcare provider if you’re unsure if your symptoms are related to menopause or another health condition.
You can have symptoms of menopause for up to 10 years before it officially occurs. The average length of menopause symptoms is about seven years. Most women say their symptoms ease up or disappear completely once they reach postmenopause.
It depends on your symptoms. For example, if hot flashes and sweating are your main symptoms, you may want to avoid warm environments or stop eating spicy foods. If you have symptoms like anxiety or insomnia, you may find that relaxing activities like yoga or reading before bed help calm your mind and lead to a more peaceful sleep.
Some women find keeping a journal of symptoms helps them identify what causes their symptoms to worsen. Then, you can take steps to avoid certain activities that make your menopause symptoms worse.
Advertisement
You’ll know you’ve reached menopause when you’ve gone 12 consecutive months without a menstrual period. Contact your healthcare provider if you have any type of vaginal bleeding after menopause. Vaginal bleeding after menopause could be a sign of a more serious health issue.
When menopause happens on its own (natural menopause), it’s a normal part of aging. Menopause is defined as a complete year without menstrual bleeding, in the absence of any surgery or medical condition that may cause bleeding to stop, like hormonal birth control, chemotherapy or radiation therapy. Surgical removal of your ovaries will result in menopause if your surgeon removes both ovaries.
As you age, your reproductive cycle begins to slow down and prepares to stop. This cycle has been continuously functioning since puberty. As menopause nears, your ovaries make less estrogen. When this decrease occurs, your menstrual cycle (period) starts to change. It can become irregular and then stop.
Physical changes can also happen as your body adapts to different hormone levels. The symptoms you experience during each stage of menopause are all part of your body’s adjustment to these changes.
The traditional changes we think of as “menopause” happen when your ovaries no longer produce high levels of hormones. Your ovaries produce the hormones estrogen and progesterone. Together, estrogen and progesterone control menstruation. Estrogen also influences how your body uses calcium and maintains cholesterol levels in your blood.
Advertisement
As menopause nears, your ovaries no longer release eggs, and you’ll have your last menstrual cycle.
There are several ways your healthcare provider can diagnose menopause. The first is discussing your menstrual cycle over the last year. Menopause is unique in that your provider will diagnose it after it occurs. If you’ve gone a full year (12 straight months) without a period, you’ve entered menopause and are postmenopausal.
Blood tests that check certain hormone levels can suggest that you’ve reached menopause. Usually, though, blood work isn’t necessary. In some situations, blood tests can be misleading because so many hormonal fluctuations occur during the perimenopause stage. Your provider may want to check hormone levels if they suspect an underlying health condition may be causing your symptoms.
Menopause is a natural process that your body goes through. In some cases, you may not need any treatment for it. When discussing treatment for menopause with your healthcare provider, it’s about treating the symptoms of menopause that disrupt your life. There are many different types of treatments for managing menopause symptoms. The main types are:
Advertisement
It’s important to talk to your provider while you’re going through menopause to craft a treatment plan that works for you. Every person is different and has unique needs. People experiencing menopause before age 40 should be offered hormone replacement therapy, except in rare circumstances (such as a personal history of breast cancer at a young age).
During menopause, your body goes through major hormonal changes — decreasing the amount of hormones it makes. When your ovaries no longer make enough estrogen and progesterone, hormone therapy can make up for lost hormones. Hormone therapy boosts your hormone levels and can help with symptoms like hot flashes and vaginal dryness. It can also help prevent osteoporosis.
There are two main types of hormone therapy:
There are risks to hormone therapy. Talk to your provider about the risks and benefits and whether hormone therapy is an option for you based on your health history, age and other factors.
Though hormone therapy is an effective method for relieving menopause symptoms, it’s not the perfect treatment for everyone. Nonhormonal treatments include things like lifestyle changes and nonhormonal medications. These treatments are often good options for women who have medical reasons to avoid estrogen, including a personal history of blood clots or receiving breast cancer treatment. Some of the nonhormonal treatments that your provider may recommend include:
Sometimes, changing what you eat can help relieve menopause symptoms. Limiting the amount of caffeine you consume daily and cutting back on spicy foods can make your hot flashes less severe. You can also eat more foods that contain phytoestrogens (nutrients that have estrogen-like properties in the human body). Foods to try include:
Certain things in your daily life may trigger hot flashes. To help relieve your symptoms, try to identify these triggers and work around them. This could include keeping your bedroom cool at night, wearing layers of clothing or quitting smoking. Maintaining a weight that’s healthy for you can also help with hot flashes.
Exercise can be difficult if you’re dealing with hot flashes, but getting regular physical activity can help relieve several other symptoms of menopause. Any type of physical activity is good for you, even yard work or swimming laps in a pool. Calm, tranquil types of movement like yoga can also help with your mood and relieve anxiety.
Talking to other women who are also transitioning to menopause can be a great relief for many people. Joining a support group can give you an outlet for the many emotions running through your head and may also help answer questions you may not even know you have. Be careful about joining groups that are not led by a menopause specialist.
There are nonhormonal prescriptions you can get from your healthcare provider that improve menopause symptoms. Some of them are:
Speak with your provider to see if nonhormonal medications could help manage symptoms.
Everyone experiences menopause differently. Because it’s so unique, there isn’t one best thing you can do for it. There are many different approaches to treating bothersome symptoms of menopause. What works for you may not work for your sister or best friend.
Talk to your healthcare provider about your symptoms and let them recommend what’s best based on your situation.
You’re at higher risk for conditions like osteoporosis and cardiovascular diseases after menopause. This is mainly due to low estrogen levels. Your healthcare provider may want to keep a close eye on your health to make sure your risk levels for these conditions isn’t too high. They may even prescribe treatment as necessary.
Osteoporosis occurs when the insides of your bones become less dense, making them more fragile and likely to fracture. Estrogen plays an important role in preserving bone mass. Estrogen signals cells in the bones to stop breaking down.
On average, you'll lose 25% of your bone mass from the time of menopause to age 60. This is largely because of the loss of estrogen. Your healthcare provider may want to test the strength of your bones over time. Bone mineral density testing, also called bone densitometry, is a quick way to see how much calcium you have in certain parts of your bones.
After menopause, your risk for cardiovascular disease tends to increase because of several things, including:
Contact your healthcare provider if symptoms of menopause are bothering you and affecting your quality of life. Most women begin the transition to menopause with mild symptoms like irregular periods or changes to their typical menstrual cycle. But symptoms can become severe and interrupt your daily life. Your provider can recommend treatments to help ease your symptoms.
Irregular vaginal bleeding can sometimes be a sign of other health conditions. Your healthcare provider may want to be sure menopause is causing your symptoms. You should contact your provider as a precaution if you have any of the following symptoms:
Some questions you may want to ask your provider include:
Yes. Until you know for sure that you’ve completed menopause, there’s a chance of pregnancy. If you don’t want to become pregnant, continue to use some form of birth control until you’re sure you’ve gone through menopause.
Yes, you can experience trouble sleeping during menopause. This can be a normal side effect of menopause itself, or it could be due to another symptom of menopause. Hot flashes are a common culprit of sleepless nights during menopause.
Yes, it can. Your declining hormone levels may affect how pleasurable sex is to you. Symptoms like vaginal dryness can make sex painful or uncomfortable. Not all women experience a decreased sexual desire. In some cases, it’s just the opposite. This could be because there’s no longer any fear of getting pregnant like there was before menopause. For many, this allows them to enjoy sex without worrying about family planning.
Don’t be afraid to talk to your healthcare provider about your sex drive or how sex feels. Your provider will discuss options to help you feel better.
It may. Hormone changes can impact your weight. For example, you may start to lose muscle as you get older, which can affect how your body gains weight.
Menopause can cause a variety of emotional changes, including:
These emotional changes can happen outside of menopause, too. You’ve probably experienced some of them throughout your life.
Your healthcare provider may be able to prescribe a medication to help you. It may also help to just know that there’s a name for the feelings you’re experiencing. Support groups and counseling are useful tools when dealing with emotional changes during menopause.
During your conversation, your provider will tell you about different treatment types and check to make sure there isn’t another medical condition causing your depression.
Andropause, or male menopause, is a term that describes decreasing testosterone levels in men. Testosterone production in men declines about 1% per year — much more gradually than estrogen production in women. Healthcare providers often debate calling this slow decline in testosterone “menopause” since it’s not as drastic of a hormone shift and doesn’t carry the same intensity of side effects. Some men won’t even notice the change because it happens over many years or decades. Other names for the male version of menopause are age-related low testosterone, male hypogonadism or androgen deficiency.
Menopause is a natural and normal part of the aging process. But knowing it’s going to happen doesn’t make it easier. The physical and emotional symptoms of menopause can be challenging and uncomfortable for many people. Fortunately, there are many treatments available to help you deal with the disruptive symptoms of menopause.
You don’t have to cope with menopause alone. Talk to your healthcare provider about the symptoms you’re experiencing and how they impact your quality of life. They can recommend treatments to manage your symptoms and make you feel better.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Menopause is natural, but it also can disrupt your life. Cleveland Clinic is here to help you get relief.
