Clinical Experience
The Cleveland Clinic Internal Medicine Residency Program allows residents to experience each of the sub-specialties of medicine in a variety of settings to help build the well-rounded internists of tomorrow. If you would like more information regarding the schedule structure and rotations available please explore the links below.
Residents not only learn from expert academic physicians, they also teach the medical students who rotate on their medicine, intensive care, subspecialty, and consult rotations. Residency programs at Cleveland Clinic have a strong relationship with Cleveland Clinic Lerner College of Medicine, Case Western Reserve University School of Medicine, and Ohio University Heritage College of Osteopathic Medicine. In addition to providing education and mentorship in the clinical setting, our residents are frequently involved with the medical students both in and adjacent to the classroom. We are proud of the teaching awards and recognition that our residents receive from medical students each year.
Community Outreach
Our residents love to have an impact on the local Cleveland community! Whether they're tackling food insecurity by organizing food drives or stocking the Cleveland Food Bank, performing screenings at local Health Fairs, biking at Velosano to raise money for cancer research, or volunteering at our Langston Hughes Women's Health Clinic, they love to make a difference. In addition, we are in the process of exploring the development of a free medical clinic specifically for unhoused patients. This initiative reflects our commitment to providing compassionate care and addressing gaps in healthcare access and quality in our community.
Curriculum/Conferences
Our innovative didactic curriculum supplements the hands-on clinical experiences that are the core of residency education. We provide engaging and interactive conference experiences that are designed for adult learners.
Resident Conferences
To maximize time and continuity in the clinical environment, we adopted an academic half day didactic model for our interns. We gather for three hours each week to host intern-led case conferences and teaching/workshops by our distinguished CCF faculty and fellows. This time is protected from all clinical obligations—no pages, no admissions, no patient appointments.
During longitudinal continuity clinic (LCC) week every 5 weeks, both seniors and interns have two half days of dedicated education that includes journal club, problem-based learning, skills workshops, simulation experiences, QI and ambulatory care curriculum.
Noon conferences provide additional opportunities for learning. To learn more about our conferences, explore below.
View a Sample Weekly Conference Schedule
- Esteemed Educator Series: Invited Department Chairs and Professors across all departments at CCF and Visiting Professors from around the country deliver noon lectures to our IM residents on their area of expertise and latest updates in the field.
- Clinical Reasoning Conference: A highly engaging conference series utilizing game-based instruction, interactive small-group discussion, and large group exercises to allow residents to reflect on clinical cases that highlight cognitive biases and examine how we think. Learn more about Clinical Reasoning Conference.
- Medicine Grand Rounds: Selected faculty and invited speakers provide both faculty and residents with updates and expertise in medicine and its subspecialties.
- Morbidity & Mortality Conference: M&M examines adverse patient outcomes to identify areas of improvement within a safe and supportive environment with the goal of improving patient outcomes.
- Journal Club: Distinguished experts review the latest literature and clinical trials. Our faculty lead discussions on investigational methods as residents design their own ideal study as a group. Finally, we review and discuss the published article to see how it stacks up.
- Intern Survival Series: A favorite for the first three months of intern year, academic half day is a dedicated crash course in inpatient medicine to kick off residency, including inpatient emergencies, common complaints, diagnostic interpretation, and the famed MICU boot camp.
- Skill Workshops: Residents hone skills with rapid fire workshops including placement of peripheral IVs/central lines, practice of office-based procedures, simulation scenarios with high-fidelity mannequins, and more.
- Board Review: In the spring we begin board review series on Tuesdays where faculty cover high yield pearls and tips for the ABIM exam.
- Mock Codes: During lighter rotations residents are called to simulation code scenarios throughout the hospital to work on practicing ACLS skills and management of commonly encountered high-acuity situations while on the wards.
Longitudinal Educational Experiences
- Contemporary Topics in Medicine: Contemporary topics in medicine is an innovative and meaningful component of the curriculum. This educational experience facilitates professional identity, hones leadership skills, and highlights the importance of humanism in medicine. We believe that learning does not happen in a vacuum. Hence, we equip residents with the skills to become effective clinician educators and word class physicians who value a holistic approach to patient care.
- Modified Problem-Based Learning: PBL’s focus is on resident-directed learning objectives derived from a clinical case in the presence of a multidisciplinary team of experts. The learning is resident led with faculty facilitation focused on building on the resident’s knowledge and skills. Learn more about Modified PBLs.
- Career Development: Residents learn how to find mentors and explore career paths as they prepare for job or fellowship applications. We provide CV review, mock interviews, personal statement workshops, fellowship director panels and more.
- Quality Improvement Curriculum: In the intern and second year, residents participate in a longitudinal, experiential quality improvement (QI) curriculum. Our residents learn QI methodology while working on quality improvement projects, largely focused in the ambulatory setting. Residents achieve excellent scholarship from this experience, including poster and oral presentations at local, regional and national meetings. Residents also have the opportunity to go through a 1-week Quality and Patient Safety elective where they discuss QI scholarship via journal clubs, learn about Root Cause Analysis (RCA), and then perform an RCA based on a real safety event at the Cleveland Clinic.
Embedded Curriculum
All inpatient rotations and most consult rotations have their own resident-specific conference series to deliver timely, high-yield topics to small groups of residents on service. On additional clinic and consult electives, our residents are invited and encouraged to attend subspecialty teaching conferences with fellows and faculty.
Research/Scholarly Activity
Scholarly Activity is a cornerstone of Cleveland Clinic's mission and an integral part of each internal medicine resident's clinical training.
We offer a robust scholarly activity program with research support and didactics which culminates in national presentations, publications, and awards.
You may read more about the scholarly activity program, research support, lectures, or annual poster session at the links below.
- Overview of Scholarly Activity Program
- Annual Resident Research Poster Session
- Scholarly Activity Lecture Series
Annual Cleveland Clinic Internal Medicine Resident Scholarly Activity Day and Reception for Poster Presentations
1 of 15-
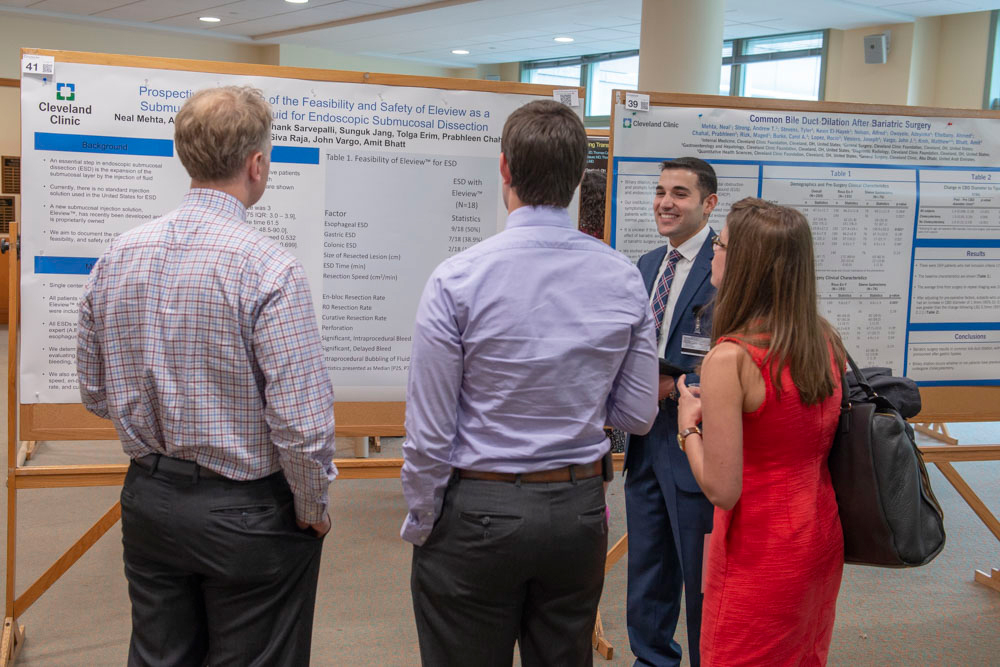
Honorable Mention Winner Presenting
-
Posters
-
Residents at Poster Session
-
Residents Together
-
Residents in Conversation
-
Resident and APD
-
Resident With His Poster
-
Resident Presenting to Colleagues
-
Resident Presenting to APD
-
Staff and Residents at Poster Session
-
Poster Session
-
APD and Residents
-
Staff Enjoying a Poster Presentation
-
Poster Presentation
-
Poster Session
Wellness
Improving and enhancing the wellness and well-being of our internal medicine residents is a priority of our residency program. We aim to ensure residents have the best possible support for avoiding burnout and depression, while enhancing work-life balance and career satisfaction. We strive to be a community which supports a culture of physical, emotional, social, and professional wellbeing. This involves fostering connections not only with our patients, but also with each other.
Current Initiatives
Physical Wellbeing
- There are multiple fitness centers that residents get free access to as a part of their training, including one on main campus within easy walking distance to the hospital.
- We work to ensure every resident has an easy way to sign up for a primary care physician in a location that works for them.
Emotional Wellbeing
- We provide an early introduction to our Caring for Caregivers resources, which can help with personal and work-related stresses in a compassionate and confidential way.
- Since the COVID19 pandemic, we have enhanced access to “boost” appointments, virtual psychiatry and more.
- We create opportunities to share gratitude and support for fellow residents and teams within the clinic.
Professional Wellbeing
- We provide representation on institute and hospital committees to continue to grow the culture of wellness and advocate for residents at every level.
Social Wellbeing
- We develop a community encouraging friendships and collegiality based upon open communication, mutual care and support.
Wellness App
To help bring everything together in one place and ensure that all residents are aware of the resources and events, we have also built a Wellness App, which acts as a hub of knowledge to share all that is available.
-
Physical Wellbeing
-
Physical Wellbeing
-
Emotional Wellbeing
-
Emotional Wellbeing
-
Professional Wellbeing
-
Professional Wellbeing
-
Social Wellbeing
-
Social Wellbeing
-
Social Wellbeing