Categorical Track
Categorical Track: The traditional residency program structure. Carried out through the 4+1 model. The residents follow a comprehensive three year curriculum to cultivate a well-rounded internist and prepare residents for the subspecialty of their choice. Residents have inpatient, consult, elective, and longitudinal clinic experiences over the course of 3 years.
4+1 Structure
The Cleveland Clinic Internal Medicine program adopted a 4+1 structure for resident schedules. All inpatient, consult, and elective rotations are assigned within 4-week blocks called X weeks followed by one week of longitudinal continuity clinic (LCC) defined as Y week. The goal of 4+1 structure is to optimize and maximize our residents’ exposure to ambulatory medicine without interfering with training in the inpatient setting.
This creates two unique opportunities:
- The ability to deliver our curriculum in a dedicated manner without interference with clinical duties
- Empowerment of our residents to be the Primary Care Physician (PCP) for their outpatient clinic patients
All categorical residents have 1 week of longitudinal continuity clinic every 5 weeks.
Structure of Y week- LCC
During the LCC week, categorical residents have:
- 6 – ½ days of their longitudinal continuity clinic
- 2 – ½ days blocked for academic time (one on Monday morning and Tuesday afternoon) which is their protected learning time
- 1 – ½ day for sub-specialty clinic of choice or additional primary care experience
- 1 – ½ day for administrative responsibilities
Structure of X Weeks- Inpatient/Consults/Electives
Primary Inpatient Rotations:
- General Medicine
- Cardiology
- Hematology/Oncology
- Liver
- Neurology
- Medical Intensive Care Unit (MICU)
- Cardiac Intensive Care Unit (CICU)
Clinic/Consult*:
- Cardiology Clinic/Consult
- Vascular Medicine Clinic/Consult
- Gastroenterology Clinic/Consult
- Renal Clinic/Consult
- General Medicine Consult
- Pre operative Clinic
- Endocrinology Clinic/Consult
- Neurology Clinic/Consult
- Pulmonary Clinic/Consult
- Rheumatology Clinic/Consult
- Geriatrics Clinic
- Infectious Disease Clinic/Consult
- Allergy/Immunology Clinic
- Women’s Health Clinic
- LGBT Clinic
- Sports Medicine Clinic
- Dermatology Clinic
- Sleep Medicine Clinic
- Palliative Medicine Clinic/Consult
*These are just a few of the clinical opportunities available at Cleveland Clinic - many residents choose to pursue elective in more specialized areas to position themselves for success in pursuing a job or applying for fellowship.
All inpatient and consult rotations have an embedded curriculum with teaching sessions arranged a few times every week by dedicated faculty in that specialty.
Three Year Curriculum
|
First Year |
Second Year |
Third Year* |
|
|
Inpatient Experience |
7 months |
6 months |
5 months |
|
Elective |
1 month |
1.5 months |
2 months |
|
Research |
0 months |
1 month |
1 month |
|
Y week LCC |
2.5 months |
2.5 months |
2.5 months |
|
Emergency Med |
0.5 months |
0 months |
0.5 months |
|
Vacation/Float |
1 month |
1 month |
1 month |
|
*All PGY3 residents attend 1 week intensive board review course in June |
|||
Clinician Educator Track (CET)
In July 2018, we proudly formed the Clinician Educator Track (CET) for the Cleveland Clinic Internal Medicine Residency Program! This track promotes the acquisition of skill needed to effectively teach, mentor and assess learners, develop new curricula, and disseminate scholarly work. This NRMP track is designed for residents interested in pursuing a career in academic medicine with a focus on medical education.
The program accepts three CET residents per year. Selection is competitive, and PGY1 residents will match into this track, separate from the categorical track.
During the CET:
- Residents have a longitudinal curriculum that spans three years.
- Residents will have one half-day of dedicated CET curriculum during their longitudinal clinic (Y) week.
- Residents have opportunities to teach built into the CET curriculum, including small group medical student teaching, inter-disciplinary teaching, teaching within GME, and also teaching at grand rounds.
- Residents have the opportunity for building curriculum and other educational projects, with time protected for this work.
- Residents will build an academic portfolio which will assist them in future endeavors.
- Residents enjoy a small team-based environment, with frequent interaction with all other CET residents and the CET directors.
Hospital Medicine Track (HMT)
Hospitalists are physicians whose primary professional focus is the general medical care of hospitalized patients. Hospital Medicine is a growing and dynamic field of Internal Medicine. Expertise in inpatient medicine includes efficiency of care for hospitalized patients, broad-based knowledge in the management of acute medical conditions, and the ability to manage and succeed in a team environment to improve patient care.
In order to meet these goals, the Internal Medicine Residency Program offers an Inpatient or Hospital Medicine Track (HMT) to give this increased focus to your training. As an adjunct to the Categorical medicine training, you will have a dedicated 10 week experience (split over second and third years). You will be exposed to concepts of quality and patient safety, care transitions, risk management, perioperative medicine, and effective consultative practice. You will also be exposed to concepts of teaching and leadership training and be introduced to medical business practices.
This track is designed for residents who are interested in Hospital Medicine careers as well as those who plan fellowship training (particularly fellowships with a strong inpatient focus).
The clinical Hospital Medicine experience will include one-to-one mentorship with a Hospitalist, following a Hospitalist work schedule. These rotations are done at Hillcrest Hospital, Marymount Hospital, or Medina Hospital, three excellent community hospitals at Cleveland Clinic. These experiences provide a unique opportunity to learn and practice Medicine in a community setting. Residents will learn clinical medicine, transitions of care, and compare the various hospital systems of care. In addition, patients in the community hospital setting often present with more “bread and butter” medical conditions, compared to many patients seen at the Main Campus tertiary care center who often have more complex situations.
The non-clinical portion of the track is comprised of a variety of educational programs and sessions. Problem Based Learning (PBL) cases are used to guide learning about several areas of systems-based practice. These sessions are supplemented with directed seminars about topics important to the practice of inpatient medicine. HMT residents spend time learning the basic concepts of Quality Improvement and Patient Safety; this experience includes the opportunity to interact with leaders in the Cleveland Clinic’s Quality and Patient Safety Institute as well as designing a QI/PS project. HMT residents also learn the fundamentals of perioperative medicine through a dedicated curriculum of case-based, didactic, and clinical experiences. A graduated experience is provided to residents in the second year of the track to build on knowledge and skills learned during the first year.
Program details
The Hospital Medicine track is designed to help physicians become effective agents of change in the complex hospital environment by training them to be leaders in coordinating and participating in the assessment, development, and implementation of system improvements. Residents will also become proficient in the care of complex hospitalized patients with exposure to:
- Increased experience in both consultative general medicine and perioperative assessment and care.
- Palliative medicine experience.
- Dedicated experience in hospital system-based competencies such as patient safety, quality improvement, and risk management.
- Dedicated experience in leadership skills including team approaches, multi-disciplinary care, management practices, and professionalism.
- Exclusive one-on-one time spent with experienced academic hospitalists and Cleveland Clinic Enterprise Senior Leadership. Hospital Medicine is a growing and dynamic field of Internal Medicine. Expertise in inpatient medicine includes efficiency of care for hospitalized patients, broad-based knowledge in the management of acute medical conditions, and the ability to manage and succeed in a team environment to improve patient care.

Kanza Qaiser, MD
Co-Director, Hospital Medicine Track
Core Faculty
Clinical Assistant Professor of Medicine

Aidan Neustadtl, MD
Co-Director, Hospital Medicine Track
Core Faculty
Clinical Assistant Professor of Medicine
Primary Care Track (PCT)
The Primary Care Track is a two-year program tailored for those passionate about pursuing a career in Primary Care. The Track has two key objectives: to provide residents with high impact clinical experiences that prepare them for independent practice in primary care and to offer unique non-clinical experiences to cultivate the growth of thought leaders in Primary Care.
PGY-1 residents are eligible to apply for the Track midway through their PGY (Post- Graduate Year) year. We welcome a maximum of 4 applicants annually. Like categorical residents, PCT residents participate in a longitudinal continuity clinic (LCC) during their Y weeks. These weeks include dedicated teaching, longitudinal clinic sessions, and the opportunity to gain experience in ambulatory clinics, either within GIM or in subspecialties that emphasize outpatient care.
In addition, PCT residents take part in the Primary Care Block (PCB) during specific months of the academic year. This includes a 5-week block in Fall and a 10-week block in spring. These blocks provide focused training in outpatient medicine through didactic teaching and exposure to subspecialty clinics that prepare residents for the complexities of GIM in ambulatory settings. The PCB includes core electives in:
- Allergy/Pulmonology.
- Cardiology.
- Dermatology.
- Endocrinology/Obesity Medicine.
- Gastroenterology/Hepatology.
- Benign Hematology/Oncology.
- Orthopedics/Sports/Rheumatology.
- Psychiatry and Psychology.
- Sleep Medicine.
- Nephrology.
- Women’s Health.
In the Primary Care Block, residents also participate in specialized workshops on leadership, patient advocacy, and practice management, and have opportunities to engage in community health initiatives. With personalized mentorship from faculty and support for scholarly work presentations at conferences, the program provides a strong foundation for residents to excel in both clinical practice and leadership roles in primary care.
The PCT program leadership and GIM clinical faculty exemplify the essence of General Internal Medicine—combining clinical knowledge, empathy, and professionalism. We are committed to developing our trainees with the skills and tools necessary for successful careers in GIM, whether in academic or community settings. Our goal is to nurture well-rounded physicians who are prepared to lead and innovate in primary care.

Sajal Akhtar, MD
Director, Primary Care Track
Core Faculty
Clinical Assistant Professor of Medicine
Preliminary Year
Preliminary residents spend the majority of the year on core Internal Medicine rotations.
The 4+1 schedule structure extends to our preliminary track as well. Instead of IM longitudinal clinic, the Y-week will consist of a clinic or consult rotation.
Sample preliminary resident schedule
Clinical experience may include
- General Internal Medicine (Kimball/Tucker)
- Subspecialty Consult Services (Nephrology, Gastroenterology, Cardiology, etc)
- Cardiology Inpatient
- Hepatology Inpatient
- Hematology/Oncology Inpatient
- Neurology
- Electives
- Emergency Department
- Vacation: 3 weeks plus a float week
VA Track
Program leadership

Megan McNamara, MD, MS
- Physician Director, Center of Outstanding Education, VA Northeast Ohio Healthcare System
- Professor of Medicine, Case Western Reserve University School of Medicine
- Physician Director, G.I.V.E. Clinic, VA Northeast Ohio Healthcare System
About the track
The VA Center of Outstanding Education (COE) track is a unique track offered by the Cleveland Clinic Internal Medicine Residency Program. We accept six physicians each year who have an interest in health care systems, quality improvement, patient safety, and interprofessional collaboration. If you are interested in this track, please make sure you select it when applying via ERAS and the NRMP Match websites (Cleveland Clinic VA Track code: 1968140C2).
Throughout your 3-year residency, your schedule will include four outpatient blocks of 12-weeks duration each. During the outpatient blocks, you will see patients in a primary care setting at the VA Northeast Ohio Healthcare System. You will be the primary provider responsible for a panel of about 200 patients. This unique opportunity provides a great deal of autonomy and unrivaled continuity. Skills and training obtained as a participant in this track will be applicable to all physicians, whether planning further specialty training or a career in primary care.
In addition to helping our residents excel in clinical knowledge, we provide an innovative curriculum to ensure our residents leave the program with the competencies in each of our six educational domains: shared-decision making, interprofessional collaboration, quality improvement, leadership, factors that influence health outcomes and professional satisfaction.
Learn more and read FAQs about the COE track.
Curriculum Overview
- Clinical training in both general medicine and subspecialties
- Didactic sessions and morning reports that address key medical topics
- Creation and implementation of Quality Improvement and Patient Safety Projects
- Interdisciplinary team-based care
- Proactive and reflective care
- Bioethics and health care humanities
Timeline
1st Year: One Block (12 weeks of primary care clinic during the second half of the year)
2nd Year: First Block (12 weeks), Second Block (12 weeks)
3rd Year: One Block (12 weeks during the first half of the year)
The remainder of your schedule will be at the Cleveland Clinic where you will do inpatient services, consults, and subspecialty clinics similar to the Cleveland Clinic residents in other tracks. You will not have any inpatient services at the VA.
During the COE blocks you will have a balanced schedule that emphasizes clinical training in primary care as well as subspecialty care, quality improvement, dedicated didactic learning time, and self-directed time to study on your own or work on research projects. A typical resident schedule for a block would be as follows:
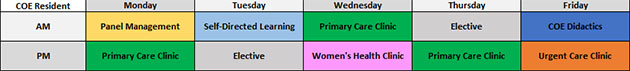
- 3 half-days of Primary Care clinic (combination of in-person and virtual appointments)
- 1 half-day of either Women’s Health or Geriatrics clinic (will have the opportunity to do both during your time)
- 0-1 half-day of either Procedure clinic, Rheumatology, Gastroenterology, or Endocrinology clinic
- 1-2 half-days of Elective time (can join subspecialty clinic at either the VA or Cleveland Clinic)
- 1 half-day of Urgent Care clinic
- 1 half-day of Panel Management
- 1 half-day of Friday Didactics
- 1 half-day of Administrative time
During elective half-day(s), residents will have the opportunity to develop close relationships with subspecialists of their choice at the VA or Cleveland Clinic. The 12-week block model allows for unprecedented continuity and opportunity to develop subspecialty skills or research.
Curriculum details
Residents undergo robust clinical training in both general medicine and subspecialties in our innovative COE curriculum. You will experience autonomy as a joint primary care physician (alternating with one other COE resident) for a panel of VA patients during a two-year period. Additionally, residents will be trained in different areas of general medicine including women’s health, geriatrics, outpatient procedures, and urgent care. Our lectures and morning reports emphasize knowledge regarding essential medical topics. We have updated our curriculum this year to emphasize training in virtual medicine in light of the COVID-19 pandemic.
Below are some examples of how we achieve our curricular objectives:
Quality improvement
- Residents receive formal training in the Lean process improvement model and work in interprofessional groups to complete a QI project. At the completion of their project, learners obtain a Lean Yellow-belt certification.
- There are weekly panel management sessions to get a bird’s-eye view of your patients, and initiate panel improvement projects to address issues such as uncontrolled hypertension or poorly managed diabetes within your panel.
Shared decision making
- Learners receive formal training in patient counseling, motivational interviewing, and communication skills.
- During their training at the VA residents have the opportunity to video-record clinic visits with their patients for analysis and direct feedback on a real patient encounter.
- Residents present challenging management cases from their panel to their colleagues to discuss various treatment approaches with other learners and providers.
Interprofessional collaboration
- Residents partner with NP residents, NP students, Pharmacy Residents, and Psychology Residents, and Social Work Residents in various projects throughout their COE training.
- As members of a primary care team, residents work collaboratively with RNs, LPNs, social workers, pharm-Ds, health psychologists, and administrative staff to manage their panel of patients.
Leadership
- Our clinical administrators and healthcare leaders at the VA provide educational sessions to our learners on their experiences in their leadership positions.
- Residents get to supervise NP students in their clinic in a dyad model that provides a great teaching experience.
- Residents are expected to direct patient management within their primary care teams. They also lead numerous sessions during our didactics including Journal Club and educational lectures.
Social drivers of health
- Our learners do Reflective Journeys during which they interact with one of their patients for part of a day within the hospital or outside in the community to better understand their healthcare and psychosocial challenges.
- During our didactics we discuss how health policy, legal precedent, societal challenges, and environmental factors affect clinical decision making.
Professional satisfaction
- The Program Leadership are always open to feedback and suggestions from our learners to implement timely and continuous improvement to the curriculum.
- Our Friday didactics occasionally include taking trips to our local Cleveland museums for unique educational opportunities.
- We emphasize residence wellness with dedicated sessions by experts, coffee breaks during several of our Friday didactics for learners to mingle freely, and ice cream parties at the end of our blocks.
Clinical Scholar Program (ClinSchoP)
The Clinical Scholar Program (CLINSCHOP) is our specialized research track for residents with a special interest in research or careers in academic medicine.
Categorical residents can apply in the winter of their PGY-1 or PGY-2 year for the next academic year. Applicants submit a personal essay, a research proposal, and letters of recommendation from both their advisors and research mentors. Submissions are reviewed by a selected group of faculty researchers and up to 8 residents are selected for the CLINSCHOP track each year.
Selected residents participate in an approximately four-month educational experience that includes clinical research courses and workshops in biostatistics, epidemiology, and medical writing, journal clubs, and research work-in-progress sessions.