Metastatic brain tumor (brain metastases) happens when cancer in one part of your body spreads to your brain. Healthcare providers treat brain metastases with surgery and radiation therapy. They may combine surgery with other treatments to minimize the brain tumor’s impact and help you maintain your quality of life.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
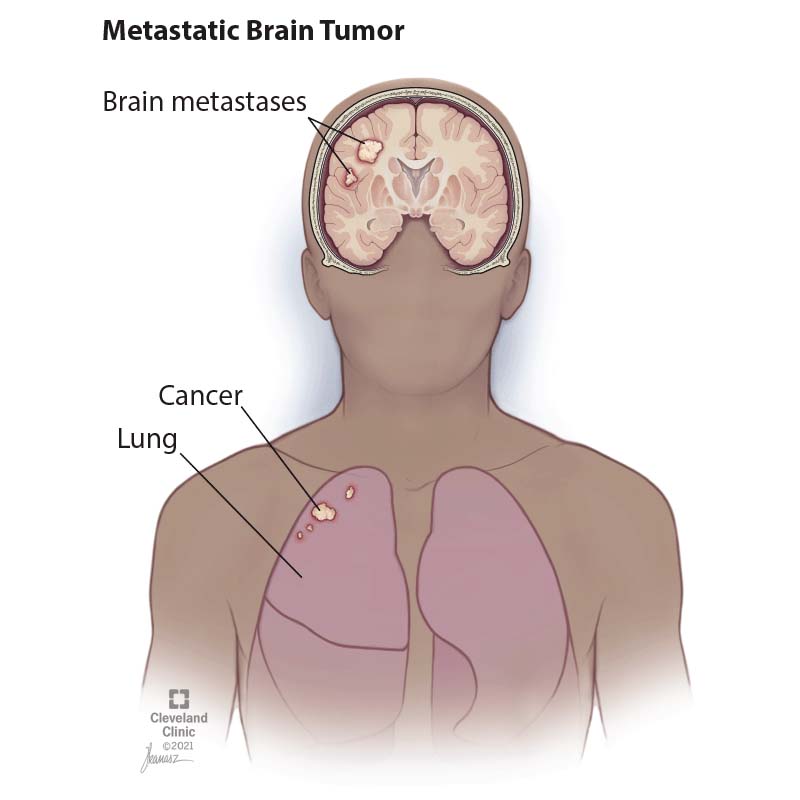
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/17225-metastatic-brain-tumor)
Brain metastases are a type of metastatic cancer. They occur when a malignant tumor in one part of your body spreads to your brain. The original tumor is called the primary tumor/cancer. Most brain metastases spread from primary cancers in your lungs, breasts or skin (specifically melanoma).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Once the cancer cells reach your brain, they form one or more new tumors. The impact the tumors have on your body depends on where the primary cancer ended up when it traveled to your brain.
Brain metastases are the most common brain tumor in adults. Experts estimate that 10% to 30% of people with cancer that starts outside of the brain will develop a metastatic brain tumor at some point. The chances of getting diagnosed increase after age 45, with most people diagnosed when they’re over 65.
Primary brain cancer, or cancer that starts in your brain, is much less common. Most tumors that start in or on your brain are benign (noncancerous).
Brain metastasis symptoms vary based on the tumor’s location and how it’s impacting your brain function in that area. The most common symptoms include:
As brain metastases progress, you may notice new symptoms, including:
Advertisement
Sometimes, brain metastases cause a stroke. But while stroke symptoms come on suddenly, most metastatic brain tumor symptoms come on slowly and worsen over time.
Metastatic brain tumors occur when cells from an existing tumor break off and spread to your brain. Usually, the cancer cells travel via your bloodstream. Researchers aren’t sure why some primary cancers are more likely to metastasize.
The most common forms of brain metastases are:
Less often, brain metastases arise from kidney cancer, colon cancer and thyroid cancer, among others.
Your healthcare provider will perform tests if you have cancer and you’re experiencing symptoms of a brain tumor. Even if you don’t have symptoms, your provider may screen you for brain metastases if you have a primary cancer that’s likely to spread.
Tests include:
Treatment for metastatic brain tumors aims to stop or slow the tumor’s growth in your brain while reducing your symptoms. Treatments include:
Your healthcare provider may begin by treating your immediate symptoms with medicine. For example, your provider may prescribe corticosteroids to reduce swelling (edema) in your brain that’s causing headaches. You may need anticonvulsants to treat and prevent seizures.
Advertisement
The most common treatments for brain metastases remove all or part of the tumor/s:
Your provider may recommend drug treatments in addition to surgery or radiation depending on your primary cancer type:
Advertisement
Brain metastases are often curable. But even when there’s no cure, treatments can help you live longer and improve your quality of life. The life expectancy associated with brain metastases was once less than six months. But new treatments have extended the timeline so that most people with this diagnosis are living longer and with much better symptom management. In fact, most people with brain metastases don’t die from their brain tumor(s).
Still, many of the questions that most people with brain metastases have — like how fast their tumor will grow — are highly individual. Your experience depends on the primary cancer, how many tumors you have and how you respond to treatment, among other things.
Your healthcare provider is your best resource for explaining how these factors inform your prognosis. Ask them about what you can expect based on your diagnosis.
Most metastatic brain tumors arise from existing lung and breast cancers and melanoma. Treating those cancers is the first step toward reducing the chance you’ll develop brain metastases. Understanding your risk for developing them is another step.
Ask your healthcare provider about your individual risk of developing metastatic brain tumors.
Advertisement
Brain metastases can create a new set of challenges when you’re already dealing with cancer treatment. But there are steps you can take (and resources you can use) to help:
Contact your provider if you’re experiencing new or worsening symptoms related to either your primary cancer or your brain metastases. Your provider needs to know about these changes so they can monitor your health and identify treatments that can help.
Brain tumors increase your risk of neurological problems that require an ER visit, like seizures or not being able to move your arms and legs. You should also seek emergency care at the first sign of a stroke. Stroke symptoms come on suddenly and include:
Having a metastatic brain tumor means you’re already coping with one kind of cancer, and you may wonder what your new diagnosis means. Here are some questions to ask your provider that can help you understand your situation:
Learning that cancer has spread to your brain may feel like a huge step into unknown territory. There are no easy answers when it comes to this diagnosis, but there is support. Don’t be afraid to ask your healthcare providers tough questions, like what outcomes you can expect from treatment and what the potential side effects may be. Your care team can guide you on your choices so you’re confident that you’re making the best ones for yourself.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When you have metastatic brain tumors, you’ll want the best care and support. Cleveland Clinic treats cancer with innovative therapies and compassion.
