A DXA scan (bone density test) is a quick, painless way to check your bone health. It’s similar to a regular X-ray, but measures the strength and mineral content of your bones instead of just taking pictures of them. Providers use DXA scans to screen you for osteoporosis, osteopenia and other conditions that can silently weaken your bones.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
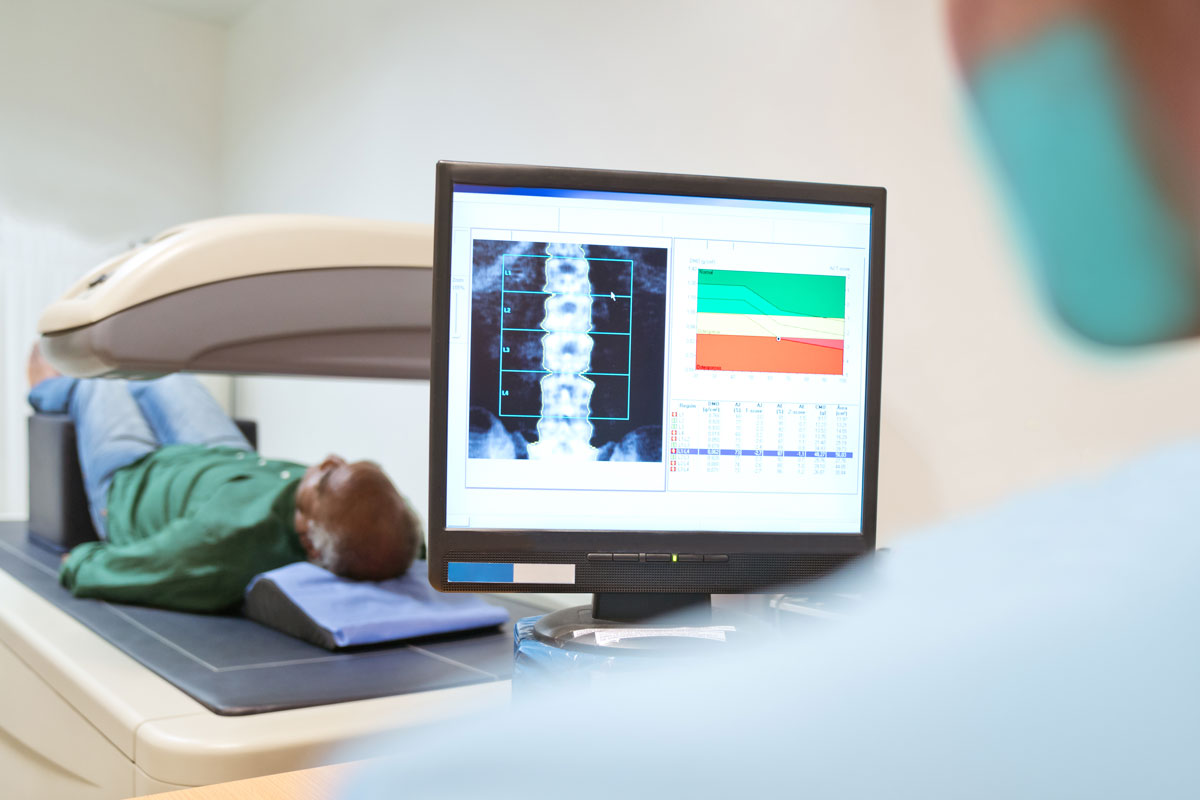
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/dexa-bone-density)
A DXA scan is an imaging test that measures the strength of your bones. It uses X-rays to measure your bone density. DXA is an abbreviation for dual-energy X-ray absorptiometry.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Healthcare providers sometimes refer to DXA scans as bone density scans, DXA scans or bone density tests. All of these are different names that refer to the same test. They used to be known as DEXA scans or DEXA tests, but healthcare providers don’t use that term anymore.
A healthcare provider might use a DXA scan to check your bones in a few situations, including to:
Your provider might use a bone density test to see how your bones have changed over time, including:
Anyone might need their bone density checked with a DXA scan. Your healthcare provider will suggest one if they want to check your bone density and fracture risk.
Some people have a naturally higher risk of developing osteoporosis and other conditions that affect their bone density. Groups who need regular DXA scans include:
Advertisement
People younger than the ages above who have an increased risk of bone loss may need regular DXA scans, too. Your provider will tell you when (and how often) you should get your bone density checked.
Some health conditions or certain medications can increase your risk for bone density issues, including:
A bone density scan uses low levels of X-rays to measure the density and mineral content of your bones. It’s similar to a typical X-ray. That’s what the X in DXA stands for.
DXA scans are outpatient procedures, which means you won’t have to stay in the hospital. There are no needles or injections in this test, and you won’t feel any pain.
You might be able to wear your regular clothes during the test, or you may have to change into a hospital gown.
Here’s how a bone density scan works:
A bone density scanner uses two types of low-level radiation to translate your bone density into pictures and graphs on a computer. Your bones will show up as white. Fat, muscles and other soft tissue will look like dark shadows in the background of the test images.
You probably won’t have to change your usual routine before having a bone density test. In general, you can:
If you take a calcium supplement or other over-the-counter (OTC) vitamins, don’t take them 24 hours before your test. Tell your provider which vitamins and supplements you take. They’ll let you know which ones you can or can’t take before a DXA scan.
You won’t be able to have a DXA scan within 24 hours of certain other kinds of imaging tests. Tell your scheduler when you’re having other tests before you make your DXA scan appointment.
A bone density test usually lasts around 30 minutes. Your test might be slightly shorter or longer depending on how many of your bones need scanning.
Advertisement
There are very few risks to having a bone density test. You won’t feel any pain or have any side effects after the scan.
You shouldn’t have a bone density test if you're pregnant. Tell your provider if you’re pregnant or think you might be pregnant. DXA scans use such a low level of radiation that they’re harmless for almost everyone, but if you're pregnant you should avoid all forms of radiation if possible.
Some studies have found that results and readings from DXA scans can vary between manufacturers of the scanning machines, but that’s not usually something you need to worry about. Your provider will monitor changes in your bone density over time and will suggest repeated or different tests if needed.
The results of a DXA scan will show how dense your bones are.
Healthcare providers use a system called a “T score” to measure your bone density. Your T score compares your bone density to a healthy, average person in their 20s or 30s. The results are measured as a negative number. The closer to zero your T score is (including being a positive number), the stronger your bones are:
Advertisement
Your provider will discuss the results with you and explain what they mean. If you have a lower-than-usual bone density, your provider will suggest treatments to help keep your bones strong, including:
DXA scans and whole-body bone scans are similar tests. Both tests involve scanning your bones, but providers use them to check different aspects of your bone health.
DXA scans are special X-rays that measure your bone density to screen you for osteoporosis and other conditions that weaken your bones.
A whole-body bone scan lets providers check to see if a cancer you might have has spread (metastasized) to your bones. You might also need a whole-body bone scan to see which cancer stage you have. They can also detect infections, lesions and other issues.
Advertisement
A DXA, DEXA or bone density scan. No matter what your provider calls it, this is a quick, easy (and painless) test. It’ll help your provider catch conditions that affect your bone density as soon as possible. You may need regular bone density screenings based on your age, family history or other risk factors you might have.
Everyone should have their bone density checked as they age. Ask your provider how often you need a DXA scan. Anyone with a family history of osteoporosis will need bone density screenings more often. Your provider will help you maintain your bone health to make sure your bones are strong enough to support you throughout your life.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
From sudden injuries to chronic conditions, Cleveland Clinic’s orthopaedic providers can guide you through testing, treatment and beyond.
