Cardioversion puts your heart back into a normal rhythm using medicines or an electric device. Providers often use cardioversion for atrial fibrillation and atrial flutter, but it also helps with other fast or irregular heart rhythms or arrhythmias. Abnormal heart rhythms can give you chest discomfort and shortness of breath.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
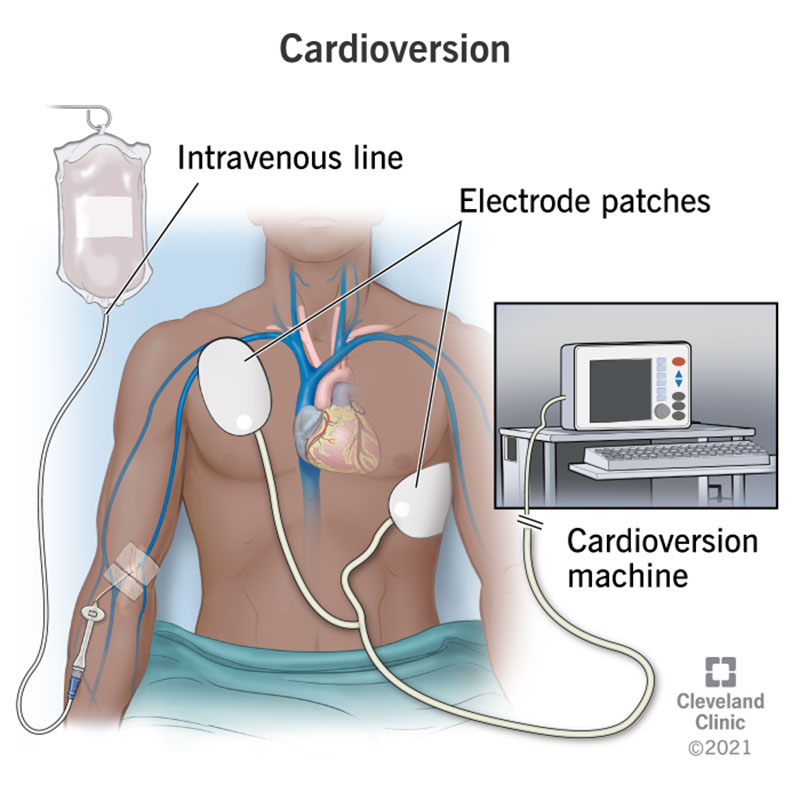
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/16952-cardioversion)
Cardioversion is a procedure your healthcare provider uses to put your heart back into a normal rhythm. They can use a device or medicine to change your heart rhythm. A cardioversion can save your life if you’re having a ventricular arrhythmia that could lead to a sudden cardiac arrest. In other cases, your provider schedules a cardioversion to prevent future problems.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Cardioversion can correct many types of fast or irregular heart rhythms, including:
You may need cardioversion to get your heart rate and rhythm back to normal so your heart can pump like it should. Abnormal heart rhythms can cause symptoms including:
Advertisement
These symptoms are signs that your heart isn’t pumping enough blood to your body. Even if you barely notice your symptoms, skipping treatment could lead to more serious problems, like a heart attack or stroke.
Your healthcare team will give you detailed instructions before your cardioversion.
You’ll need to make plans to have someone come with you to drive you home. You won’t be able to drive for 24 hours after your procedure.
Ask your provider how you should take your blood thinners/anticoagulants, such as warfarin (Coumadin® or Jantoven®), and your diabetes medications or insulin on the day of your cardioversion.
Unless your provider tells you otherwise, take all other regular medications as scheduled. Take them with small sips of water on the day of your cardioversion.
Eat a normal meal the evening before your procedure. DO NOT eat, drink or chew anything after midnight before your procedure. This includes gum, mints, water, etc.
Be careful not to swallow any water when you brush your teeth.
You’ll want to keep it simple on the day of your procedure.
Bring a complete list of your medicines and a one-day supply of your prescription medications. Don’t take these medications without talking with your provider first.
You’ll lie on a bed, and your provider will start an intravenous (IV) line in your arm or hand. They’ll give you medications and fluids through the IV during the procedure in the electrophysiology (EP) lab.
They’ll put electrocardiogram (EKG) patches and adhesive cardioversion pads on your chest, and possibly your back. If there’s hair in the way, they’ll shave it.
You may need to have a transesophageal echocardiogram (TEE) before your cardioversion. Your provider will numb your throat and put a thin tube with a transducer into it. The transducer creates pictures of your heart to check for blood clots that could come loose during the procedure.
No. You’ll get medication through your IV to make you fall asleep during the procedure.
While you’re asleep, your provider will use the cardioverter machine (defibrillator) to quickly deliver specific amounts of energy to your heart through the cardioversion pads. The shock interrupts your abnormal electrical rhythm and restores a normal heart rhythm. It may take several shocks to get your rhythm back to normal, but it won’t be painful as you’ll be asleep.
Advertisement
During your cardioversion procedure, your provider will monitor your oxygen level, heart rhythm and blood pressure. They’ll use the following equipment:
The procedure itself lasts only a few minutes. However, you should plan to spend about four to six hours total to allow time for procedure preparation and your recovery.
You‘ll slowly wake up after the procedure. You’ll be drowsy from the medication your provider gave you during the procedure. Your chest may be tender for a few days. Hydrocortisone cream can give you some relief.
Once you’re fully awake, your healthcare provider will talk to you about your procedure results and your plan of care. Be sure to ask your provider if you should keep taking the same medications you took before the procedure. You may need to take medicine to keep an abnormal heart rhythm from happening again.
Advertisement
When you move to the recovery area, you can have something to eat and drink, and your family can visit. You may have an EKG before you go home. Your provider will keep checking your blood pressure and heart rhythm.
Your provider will tell you which over-the-counter medications you can take for pain relief if needed. Let them know about any symptoms that are severe or last a long time. You may need to take medicines to prevent abnormal rhythms and/or blood clots.
No. You will likely go home the day of the procedure.
No. For your safety, a responsible adult must drive you home. You won’t be able to drive for 24 hours after the procedure.
Cardioversion returns your heart rhythm to normal and cuts down your symptoms. Also, your heart may work better after cardioversion.
Complications don’t happen often. They include:
You’ll most likely go home the same day as your cardioversion. However, you can’t drive for 24 hours because you’ll be sleepy from the anesthesia. You’ll be able to eat and drink after your procedure. Ask your provider when you can go back to work.
Advertisement
You’ll need to keep your follow-up appointments with your provider so they can see how well you’re responding to treatment. They’ll also want to see if you’re on the right dose of any medicines they prescribed for you. Tell your provider if you start having symptoms again.
Cardioversion is only one part of your plan of care. It’s also important for you to take your medications, live a heart-healthy lifestyle and keep your follow-up appointments. Talk to your provider if you have any questions or concerns.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When your heart rhythm is out of sync, the experts at Cleveland Clinic can find out why. We offer personalized care for all types of arrhythmias.
