A pericardiectomy is a surgical procedure to remove all or part of your pericardium, or membrane sac around your heart. A normal pericardium protects your heart, but a stiff pericardium can’t stretch enough. This leads to heart failure symptoms. A pericardiectomy can give many people years of symptom-free life.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
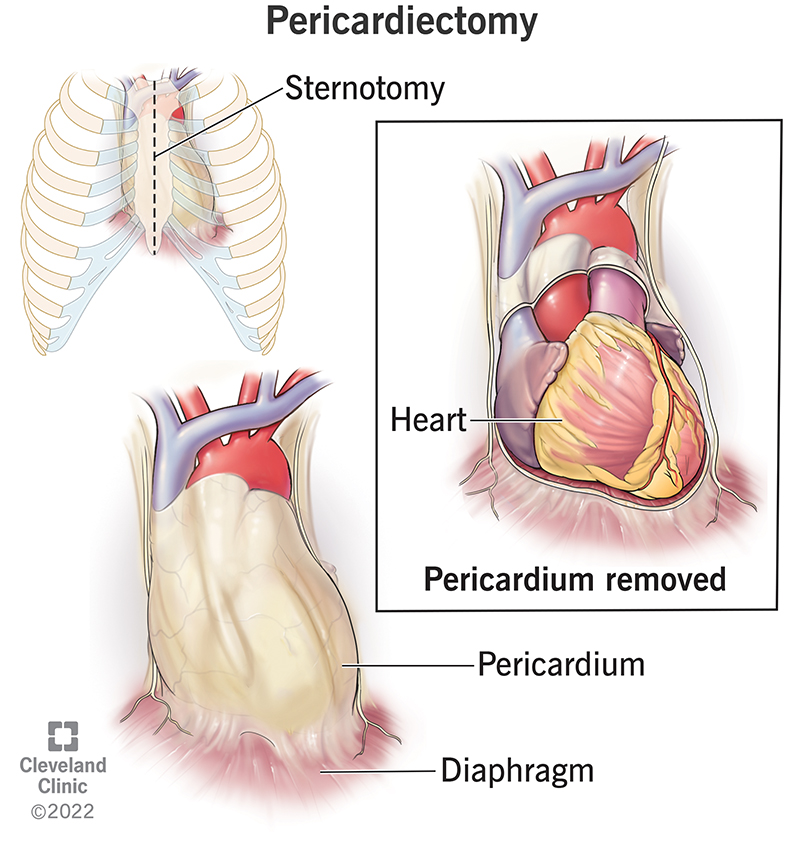
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17352-pericardiectomy)
A pericardiectomy, sometimes called “pericardial stripping,” is the surgical removal of part or all of your pericardium. The pericardium:
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Yes. The pericardium isn’t essential for normal heart function. Removing the pericardium doesn’t cause problems as long as your lungs and diaphragm (the large muscle below your lungs) are intact.
If you have pericarditis, your pericardium already has lost its lubricating ability. Removing it doesn’t make that worse.
The most common reason for performing a pericardiectomy is constrictive pericarditis, a condition in which your pericardium becomes stiff and possibly calcified.
This stiffness prevents your heart from stretching as it normally does when it beats.
Then:
For the most advanced cases of constrictive pericarditis, surgical treatment is the best option.
Constrictive pericarditis causes include:
Advertisement
Pericardiectomy also treats people with:
Pericardiectomies are rare surgeries. Even a hospital that does more pericardiectomies than most may only have 30 to 50 cases per year.
About 20% of people with constrictive pericarditis in the United States end up getting a pericardiectomy.
Your healthcare team will make sure equipment is ready for a safe operation. Most often, your surgeon will use cardiopulmonary bypass (the heart/lung machine). This allows them to safely remove the pericardium from the sides and back of your heart.
Your surgical team will:
Yes, pericardiectomy is usually open-heart surgery. -This allows your surgeon to get to your heart to remove your entire pericardium. Surgeons prefer this to a partial pericardiectomy technique.
Some surgeons may use a thoracotomy approach, which means they make a cut between your ribs to get to your heart.
On average, a pericardiectomy takes about two to three hours. However, some people have more than one procedure while they’re in the operating room.
You will feel sore when you wake up after your surgery. You will have one or more tubes draining extra fluid from your chest.
You’ll probably be able to drink liquids the day after surgery and eat food later.
Most people will continue to take a diuretic after surgery, but in lower doses, than they needed before surgery.
Advantages of a pericardiectomy include:
Pericardiectomy is a major cardiac surgery procedure. To minimize risks, choose a cardiac surgeon experienced in the procedure.
Pericardiectomy risks include:
People with prior heart surgery, major medical conditions or a history of radiation have a higher risk of pericardiectomy complications.
Advertisement
A small number of people still have symptoms after surgery.
Most people who have a pericardiectomy surgery stay in the hospital for five to seven days.
You can go back to your normal activities when you get home, except for lifting.
Full recovery after pericardiectomy takes six to eight weeks, depending on how serious your condition was before the surgery. For the most serious cases, recovery can take longer than eight weeks.
People with severe pericardial constriction who don’t have other heart or lung diseases often feel better immediately after surgery. Most people notice a significant improvement by six to eight weeks and gradually keep improving for a while.
The long-term outlook after pericardiectomy surgery depends on the cause of your constrictive pericarditis. Studies have found that people with idiopathic (unknown cause) constrictive pericarditis had the highest long-term survival.
Outcomes tend to be better in people who:
Scar tissue will form around your heart after pericardiectomy and may form between your heart and surrounding structures such as your lungs and diaphragm. This makes future heart surgeries somewhat challenging — but not impossible — for experienced cardiac surgeons.
Advertisement
Without treatment, the survival rate of constrictive pericarditis is low. After a pericardiectomy, 78% of people can live five years and 57% live another 10 years.
It depends on several factors, including:
About 80% of people who had a pericardiectomy after constrictive pericarditis with an unknown cause were alive five to seven years after the surgery. However, for people who got constrictive pericarditis from chest irradiation and had a pericardiectomy, up to 30% survived five to 10 years.
Contact your provider if you have:
You should see your cardiologist one or two weeks after you leave the hospital. You also should have an echocardiogram six weeks after surgery and then as often as your provider recommends. An echocardiogram is an ultrasound of your heart that allows your cardiologist to see how well your heart is pumping.
Pericardiectomy is a surgery that removes part or all of your pericardium.
Pericardiocentesis uses a needle to drain extra fluid from your pericardium.
Both are surgeries. Pericardiectomy removes your pericardium. Pericardiotomy just makes a cut in your pericardium to drain fluid.
Advertisement
It may feel scary to know you need to have a pericardiectomy but talk with your healthcare provider about any concerns you have. Before you leave the hospital, make sure you understand what you’re supposed to do at home. Don’t be afraid to ask questions if you need more information. Your healthcare provider may give you medicines to take, exercises to do or limits on what you eat. Following these instructions will help your recovery.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Whether your pericardial disease comes on acutely without warning or is chronic, Cleveland Clinic has the best treatments for this heart condition.
