Lymphedema is swelling that happens when something affects your lymphatic system. Lymphedema often affects your arms and legs, but may also affect other areas of your body. Healthcare providers can’t cure lymphedema, but they can ease its symptoms.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
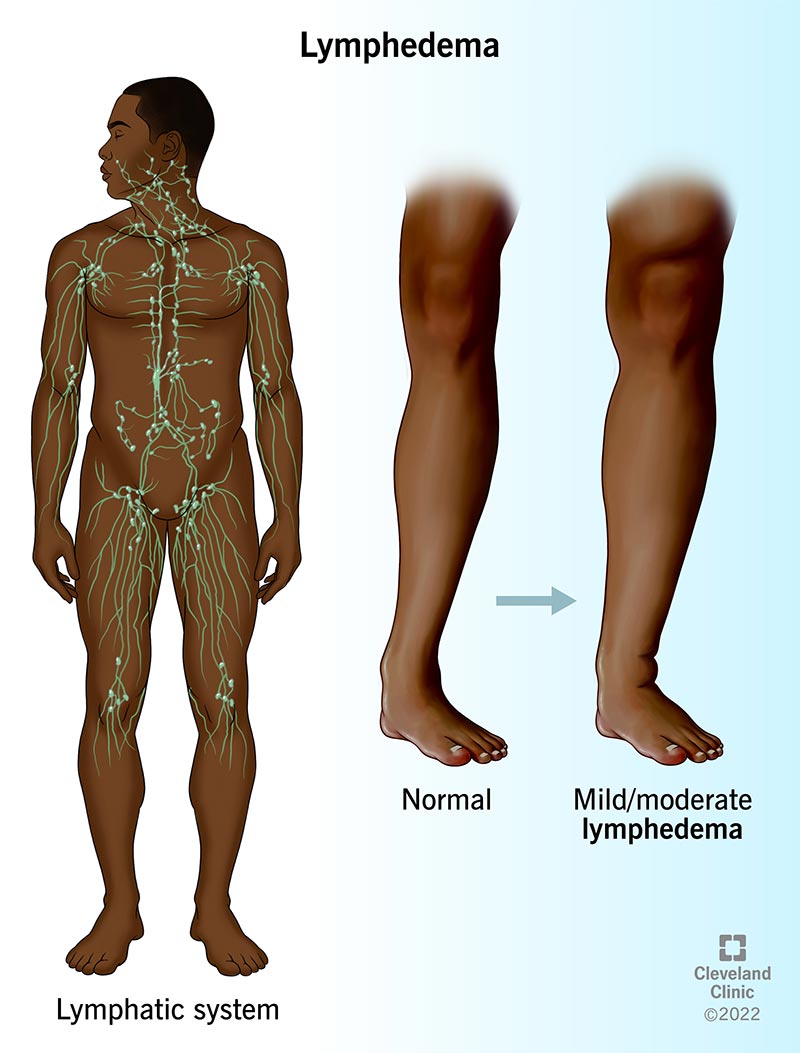
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/8353-lymphedema)
Lymphedema is swelling in various areas of your body that happens when something affects your lymphatic system. Your lymphatic system collects excess fluid, proteins and toxins from your cells and tissues and returns them to your bloodstream.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
When your lymphatic system doesn’t work well, your body accumulates fluid and may begin to swell. The swelling typically affects your arms and legs, but it can affect other areas of your body, too. Lymphedema also increases your risk of developing an infection where you have the condition.
This can happen after certain surgeries or because you have certain medical conditions or genetic conditions. You may develop lymphedema spontaneously, meaning it happens for no known reason.
Lymphedema symptoms may be mild, causing minor swelling and discomfort. Sometimes, however, lymphedema may cause significant swelling that can be painful and cause skin issues such as infections and wounds. Healthcare providers can’t cure lymphedema, but they do have treatments to reduce swelling and discomfort. There are also many things you can do to limit the impact lymphedema may have on your quality of life.
If you have lymphedema, your arms, legs, feet and other areas of your body may look and feel swollen. Lymphedema can be painful and may affect your ability to manage daily activities. Many people with lymphedema feel self-conscious about the ways it changes their appearance.
It can be. If you have lymphedema, you may be at risk of developing infections that start in your skin. These infections may be life-threatening. Rarely, lymphedema may also lead to lymphangiosarcoma, a very rare skin cancer.
Advertisement
Yes, there are two types of lymphedema — primary and secondary.
Primary lymphedema comes from rare, inherited conditions that affect how your lymphatic system develops. Primary lymphedema affects about 1 in 100,000 people in the U.S. Lymphedema from these conditions can appear at these ages:
Secondary lymphedema may happen if your lymphatic system is damaged from surgery, trauma or radiation therapy. It is most common in people who’ve had breast cancer treatment. That said, not everyone who has breast cancer treatment develops lymphedema.
No, it’s not a form of cancer.
The most common symptom is swelling. Swelling may develop slowly. You may not notice unusual swelling in lymphedema’s early stages. Swelling from lymphedema may also come on suddenly. Other lymphedema symptoms you may notice include:
Several things may cause lymphedema, including:
Advertisement
If you have swelling that may be due to lymphedema, your healthcare provider may do several tests to determine if lymphedema is causing the swelling. Those tests may include:
Yes, healthcare providers use the following staging system:
Advertisement
There’s no cure for lymphedema, which means you can’t get rid of it. There are many different ways to treat lymphedema so it doesn’t affect your quality of life.
Lymphedema treatments vary depending on your condition’s cause and stage. Treatments may include physical therapy or other treatment to keep lymphatic fluid moving and reduce swelling and pain. Your healthcare provider may also prescribe antibiotics for infections or pain medication.
Lymphedema treatment typically includes a combination of physical therapy and garments or bandaging that moves fluid from areas affected by lymphedema. If you have physical therapy for lymphedema, it’s very important to use garments or bandaging after therapy to maintain the treatment’s effect. Physical treatments for lymphedema may include:
Advertisement
Healthcare providers may recommend surgery if nonsurgical treatments haven’t helped your symptoms. It’s done at centers that specialize in this treatment. Lymphedema surgery is usually only done if your lymphedema is severe. It isn’t a complete cure either. Not everyone can have surgery. If you have lymphedema, ask your healthcare provider if surgery makes sense for you. Surgical treatments may include:
Lymphedema is a chronic condition. Treatment and lifestyle changes don’t cure lymphedema but they’re effective ways to manage lymphedema symptoms.
You can’t reduce all lymphedema risks, but there are things you can do to reduce and possibly prevent swelling. If you’re having breast cancer surgery or other treatment, ask your surgeon and other healthcare providers about exercises that may reduce swelling. Other steps include:
It can be hard to get comfortable when your arm or leg is swollen. These suggestions may be helpful:
Contact your healthcare provider if you notice your affected arm or leg is more swollen or if you think you have an infection.
While there’s no cure for lymphedema, making small changes in how you go about your day may help reduce swelling and other symptoms. Small changes to consider include protecting against infection, getting exercise and making small changes in your diet.
Lymphedema puts stress on your skin, making it more vulnerable to infection from injuries like cuts, scrapes and scratches. Infections may create serious medical issues for people with lymphedema. You can help protect yourself by practicing good hygiene and protecting your skin. Suggestions include:
Lymphedema happens when fluid gathers in one spot in your body. Exercise is one of the best ways to keep fluid moving. Talk to your healthcare provider before starting an exercise routine. They’ll have suggestions and may recommend special exercises you can do. Other suggestions are:
Healthy eating habits may help you control swelling. Your lymphatic system is more effective when it’s powered by nutrients from fruits, vegetables, whole grains and lean protein. Healthy eating also helps you maintain a weight that’s right for you. Some suggestions include:
Lymphedema is swelling in various areas of your body that happens when something affects your lymphatic system. It’s a chronic condition that may take a toll on your health, your spirits and your self-esteem. Lymphedema is a tough condition. But you can take steps to control your symptoms and make it easier to live with lymphedema. Small changes such as eating a healthy diet and adding exercise can make a big difference. Your healthcare provider can also recommend treatments to ease lymphedema symptoms. Let them know if you’re having trouble living with lymphedema. They’ll give you the help you need or point you in the right direction to find that help.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s primary care providers offer lifelong medical care. From sinus infections and high blood pressure to preventive screening, we’re here for you.
