Eczema is a skin condition that causes dry and itchy patches of skin. It’s a common condition that isn’t contagious. Symptoms of eczema can flare up if you contact an irritant or an allergen. There are treatments available to help you manage symptoms, but there isn’t a cure.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Eczema is a condition that causes your skin to become dry, itchy and bumpy. This condition weakens your skin’s barrier function, which is responsible for helping your skin retain moisture and protecting your body from outside elements.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Eczema is a type of dermatitis. Dermatitis is a group of conditions that cause skin inflammation.
There are several types of eczema. Each type has unique triggers that can affect your skin’s barrier function, including:
It’s possible to have more than one type of eczema at the same time.
Eczema can affect anyone at any age. Symptoms usually appear during childhood and last into adulthood. You might be more at risk of having eczema if you have a family history or a diagnosis of:
Eczema is common and affects more than 31 million Americans. Infants are prone to eczema, and 10% to 20% will have it. However, nearly half of all infants diagnosed with eczema outgrow the condition or have significant improvement as they get older.
The first signs of eczema are itchiness, dry skin and a rash. These signs indicate that you came into contact with a trigger in your environment that caused your symptoms to start or flare up. Identifying environmental triggers and avoiding them can reduce your risk of an eczema flare-up in your future.
Symptoms of eczema include:
Advertisement
Eczema can look different on each person diagnosed with the condition. If you have a dark skin tone, an eczema rash can be purple, brown or gray. If you have a light skin tone, an eczema rash can look pink, red or purple.
Symptoms of eczema can show up anywhere on your skin. The most common places where you’ll notice symptoms of eczema include on your:
While less common, eczema can also occur on your:
Eczema doesn’t usually cause pain. If you scratch your skin, you could break the surface of your skin and create a sore, which could be painful. Some types of eczema, like contact dermatitis, cause a burning sensation and discomfort.
Several factors cause eczema, including:
Eczema affects each person diagnosed with the condition differently. What causes your symptoms to flare up might not trigger someone else with the condition. Common triggers that cause eczema include:
The connection between eczema and food allergies is unclear. If you have food allergies, then one of the reasons why you must avoid that food is that it may cause or worsen your eczema symptoms. Examples of common allergies include:
Pay attention to what you eat. If your eczema flares up after you eat a certain food, then you might have an allergy to it. If you don’t have a food allergy, then there are no foods that will cause or worsen your eczema.
While eczema can cause your immune system to overreact, it isn’t classified as an autoimmune condition. Research is ongoing to learn more about how eczema interacts with your immune system.
No. Eczema isn’t contagious. You can’t spread eczema through person-to-person contact.
A healthcare provider will diagnose eczema after a physical exam, where they can take a close look at your skin. Most often, people receive an eczema diagnosis as a child, as it’s common among children, but a diagnosis can happen at any age when symptoms arise.
Advertisement
Symptoms of eczema can look similar to other conditions. Your provider might offer tests to rule out other conditions and confirm your diagnosis. Tests could include:
Your healthcare provider might ask the following questions to learn more about your symptoms, including:
A primary care provider may recommend you visit a dermatologist to diagnose and treat your eczema. A dermatologist specializes in skin conditions.
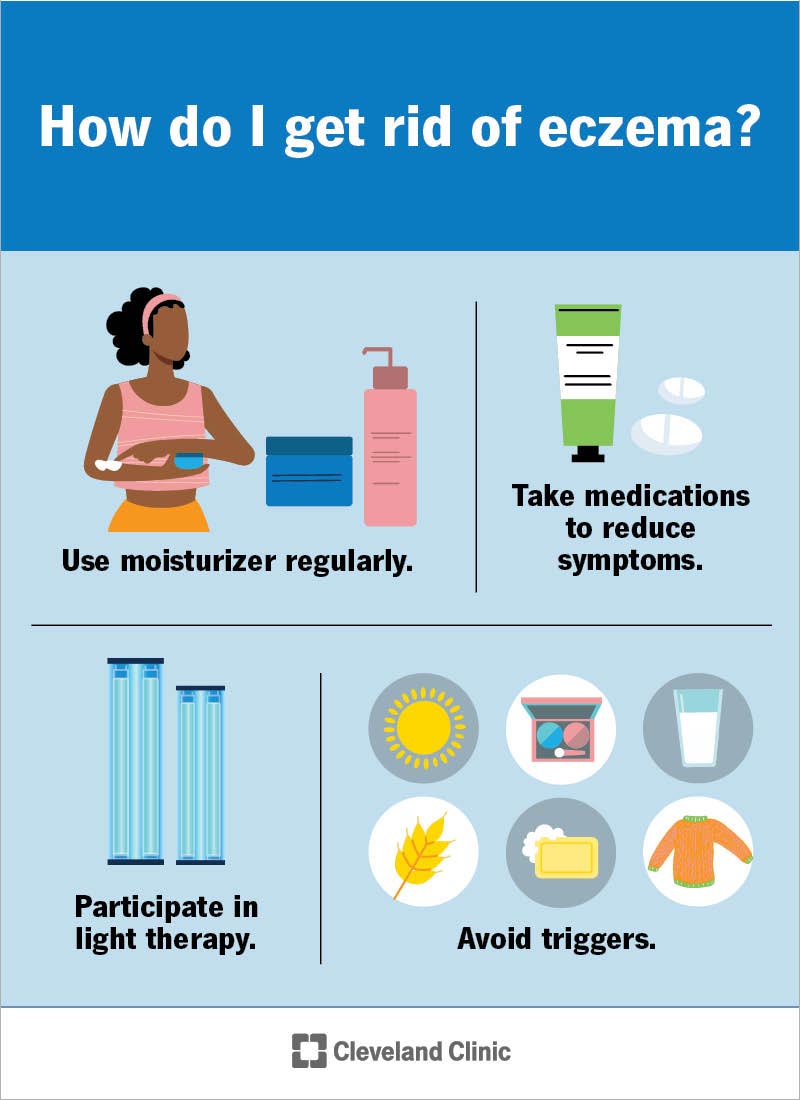
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/9998-eczema)
Your treatment for eczema is unique to you and what caused your symptoms to flare up. Treatment for eczema could include:
Advertisement
If your child has skin issues, such as eczema, you can:
There are several options of moisturizer available to treat eczema. Choose skin care products that:
It may take several different products through trial and error before you find one that works for you. If you need help choosing a moisturizer, talk to your healthcare provider.
Treating and managing eczema can be difficult if the cause is something you can’t control, like genetics. Fortunately, you may have some influence over your environment and stress levels. Do your best to figure out what triggers or worsens your eczema, and then avoid it. The goal is to reduce itching and discomfort and prevent infection and additional flare-ups.
Advertisement
After treatment, it could take several weeks before your skin clears up completely. Topical medications or oral medications prescribed by your healthcare provider help your symptoms go away faster. If your symptoms get worse after treatment, or if they don’t clear up after a few weeks, contact your provider.
Complications are possible with eczema and could include:
Symptoms that are a sign of complications include:
Eczema and other types of dermatitis aren’t harmful to the rest of your body. The condition isn’t deadly. Nearly half of children with eczema outgrow the condition or experience improvement by the time they reach puberty. Others will continue to have some form of the condition throughout their life. For adults with eczema, the condition can be well managed with a good skin care routine.
Eczema can be a lifelong condition. It can start in infancy and continue through adulthood. You can manage your symptoms with at-home remedies, over-the-counter medications and prescription medications.
No, there isn’t a cure for eczema. There are treatments available, but no treatment can eliminate your symptoms 100% of the time. Eczema is a chronic condition, which means it can go away and come back unexpectedly. Treatments are very effective in reducing the symptoms of itchy, dry skin.
There are steps you can take that may prevent eczema flare-ups and outbreaks, including:
Many people live with eczema, and it can be challenging. But there may be times when your eczema disappears. This is known as a “remission” period. Other times, you may have a “flare-up,” which is when your symptoms show up or get worse. The goal of treatment is to prevent flare-ups and your symptoms from getting worse. Be sure to avoid triggers, moisturize, take your medicine and follow your healthcare provider’s instructions.
Visit your healthcare provider or your dermatologist if:
Yes, certain temperatures or weather patterns can affect your skin and can make eczema worse. Low humidity (dry air) in the winter months can dry out your skin. Humidity caused by high heat can make you sweat, which can make your itchiness worse.
Eczema is a very common and uncomfortable skin condition. It can affect your quality of life. At its worst, it can keep you from sleeping, distract you and make you feel self-conscious in public. See a dermatologist or healthcare provider as soon as you start to see signs of eczema. Explore at-home remedies and prescription treatments until you find the best remedy for your skin.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Every day, people see your skin, hair and nails. At Cleveland Clinic, our expert and caring dermatology team will make sure they’re healthy and strong.
