Sepsis is a life-threatening reaction to an infection that causes your immune system to harm healthy tissues and organs. It can develop quickly and lead to organ failure or death without urgent care. Recognizing the symptoms and getting medical help right away could save your life.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_0xbzmf36/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Learn what sepsis is and why it’s important to receive treatment quickly.
Sepsis is your body’s overwhelming response to an infection. It happens when an infection you already have triggers a serious chain reaction throughout your body.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
When you have an infection, your immune system normally tries to fight it. But sometimes, your immune system overreacts. It starts damaging healthy tissues and organs by mistake. This can cause widespread inflammation throughout your body.
Sepsis is a life-threatening medical emergency. Without urgent treatment, it can lead to tissue damage, multiple organ failure and death.
Sepsis can lead to septic shock, which can cause death in as little as 12 hours.
Healthcare providers used to organize sepsis into three distinct stages: sepsis, severe sepsis and septic shock. Now they divide the condition into sepsis and septic shock. They use the number of organs damaged by sepsis to indicate its severity.
Bacteremia means you have bacteria in your bloodstream. Sepsis occurs when your immune system overreacts to an infection. It attacks healthy tissues, causes inflammation and can be life-threatening.
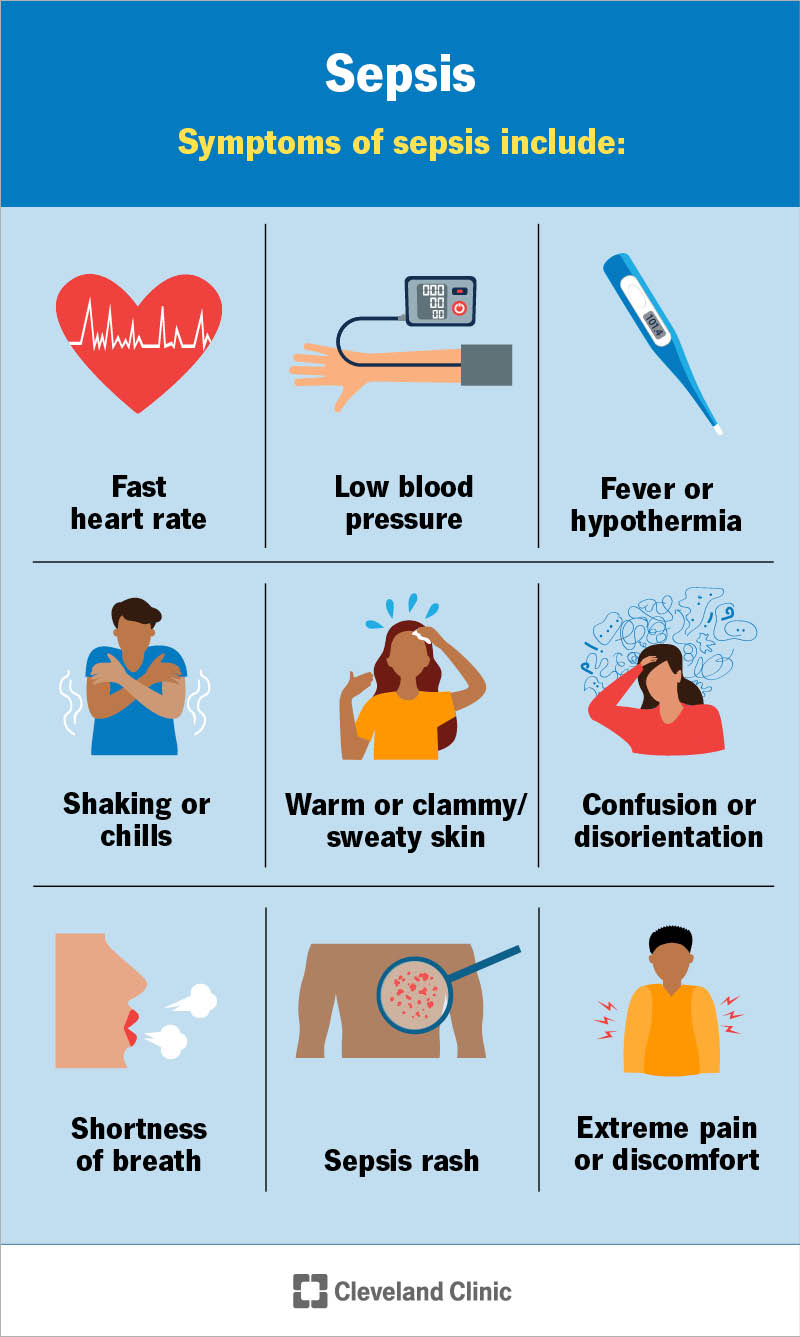
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/12361-sepsis)
Sepsis can affect many different areas of your body. So, there are many possible symptoms. If a bloodstream infection (bacteremia) triggered the condition, you may develop a sepsis rash. The rash makes your skin appear red or discolored. You may see small, dark-red spots on your skin.
Other common signs of sepsis include:
Advertisement
Bacterial infections are the most common cause of sepsis. Fungal, parasitic and viral infections are also potential sepsis causes. You can get sepsis when an infection triggers a chain reaction throughout your body that causes organ dysfunction.
The infection leading to sepsis can start in many different parts of your body. Common sites and types of infections that can lead to sepsis include:
Sepsis itself isn’t contagious — you can’t spread it to other people. But you can spread the infections that can cause sepsis.
Sepsis can affect anyone. But you’re more likely to develop it if you:
Newborns and infants are another at-risk group.
If you have an infection or bacteremia, a healthcare provider may quickly assess your risk of developing sepsis and dying from it. Providers use various sets of sepsis criteria to figure out your risk of death and how urgently you need treatment.
Some healthcare organizations use alert systems or artificial intelligence (AI) to find sepsis symptoms hours before traditional tests.
After the provider assesses your risk, they may confirm a sepsis diagnosis using a combination of findings. They’ll perform a physical exam and evaluate your symptoms. Then, they’ll order tests to identify the infection and any organ damage or dysfunction. These tests may include:
Yes. With early diagnosis and treatment, sepsis is curable. But many factors can affect your prognosis (outlook), including your overall health and the severity of the condition.
Advertisement
Sepsis treatment needs to start immediately. If your provider diagnoses you with the condition, they may send you to the intensive care unit (ICU) of the hospital for special treatment.
Sepsis treatments may include:
If you survive sepsis, you’ll more than likely need rehabilitation before returning home. Your body has been through a lot. Healthcare providers will help restore your health. You’ll slowly learn how to take care of yourself again.
Even just sitting up and standing may be hard at first, depending on your condition. You’ll work with a provider to get your body up and moving. You’ll practice getting yourself to the bathroom and bathing yourself. Once you’ve regained your strength and restored your mobility, you’ll be able to go home.
Advertisement
You’ll need to give your body and mind time to recover. When you get home, you may have some unpleasant symptoms. Some people develop a condition called post-sepsis syndrome. Physical effects may include:
Mental and emotional effects may include:
You’re also at a higher risk of developing sepsis again. So, make sure to have any new infections treated immediately.
Your healthcare provider will help you develop a plan to continue in your recovery. At first, you’ll work on small, achievable goals like bathing and dressing. You’ll work to rebuild your physical strength. But it’ll also be important to take care of your mental health. Talk to your family, friends and providers about how you’re feeling. It’ll take some time. But eventually, you should start to feel like yourself again.
With quick diagnosis and treatment, many people with mild sepsis survive. Without treatment, most people with the most advanced stage of sepsis (septic shock) will die. Even with treatment, up to half of all people with septic shock will die.
Advertisement
Many people die in the months and years after surviving sepsis. But researchers don’t know if the increased risk of death is due to previously having sepsis or having an underlying health condition.
Because of this and other factors, research studies show varying rates of life expectancy after sepsis. These rates range widely. But they typically show that more than half of all sepsis survivors die within five years.
But each case is unique. Stay in close contact with your healthcare team so you can catch any health issues early.
Steps you can take to help prevent sepsis include:
Sepsis is serious, but knowing the signs and acting fast can save a life — maybe even your own. If you have an infection and something doesn’t feel right, listen to your body. A high heart rate, confusion or fast breathing can be early signs that something more is happening.
Getting medical help right away gives you the best chance to recover and heal. Trust your instincts — they’re one of your strongest tools.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Have a virus, fungus or bacteria? Some of these “bugs” won’t go away on their own. Cleveland Clinic’s infectious disease experts are here to help.
