Sarcoidosis is a condition that causes lumps or nodules (granulomas) to form in your lungs, lymph nodes, skin, eyes and other parts of your body. Symptoms include cough, shortness of breath, tender sores on your shins, eye pain and redness. Many cases go away on their own or with treatment, but sometimes it becomes a chronic condition.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
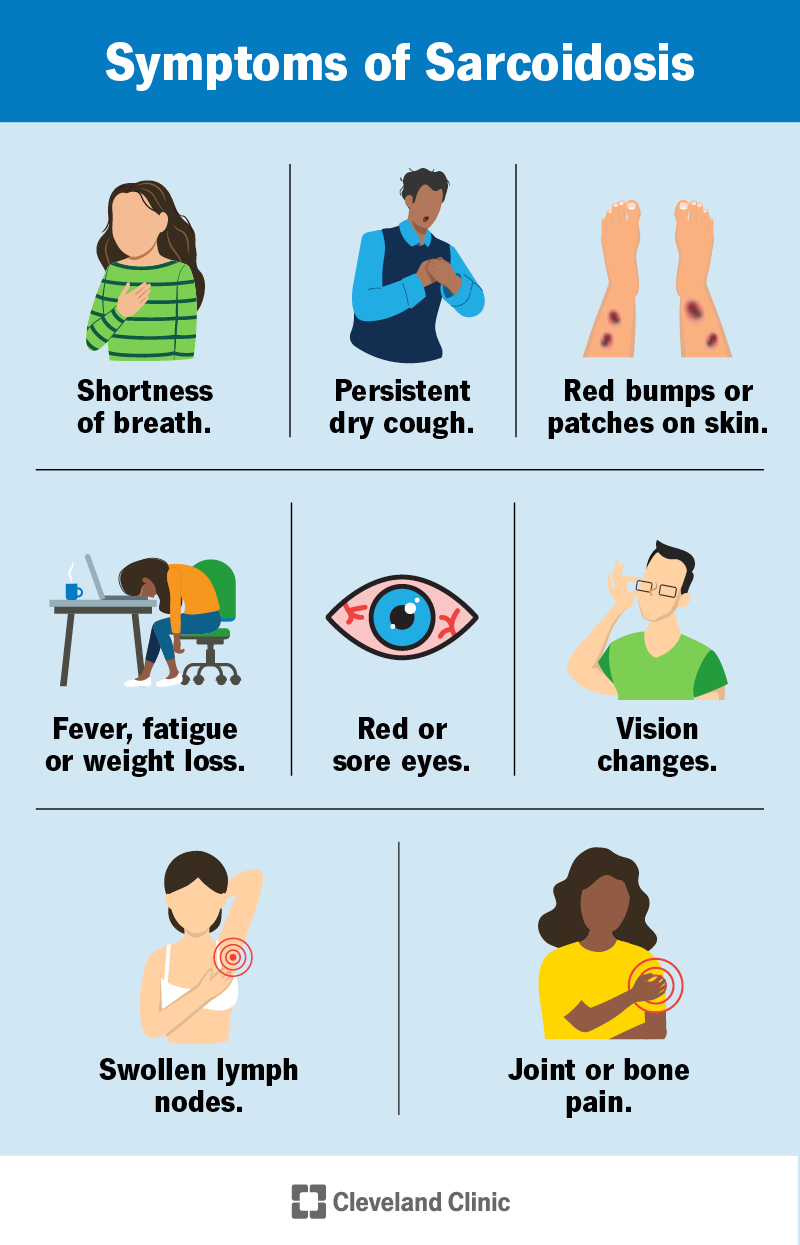
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/11863-sarcoidosis)
Sarcoidosis is a condition that causes your immune system to overreact and make lumps or nodules called granulomas. Depending on location and size, granulomas can cause mild to severe symptoms or no symptoms at all. In some cases, they can turn into fibrosis, causing permanent lung scarring.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Granulomas can be found almost anywhere in your body, but they’re most commonly found in your lungs or lymph nodes. You may also have noticeable symptoms of granulomas in your skin, eyes or muscles.
A granuloma is an area of inflammation caused by your immune system. It’s made up of a cluster of white blood cells that have been “walled off” from the rest of your body to try to protect you from something your immune system thought was harmful. Granulomas are surrounded by fibrous (dense) tissue, which makes them feel hard and lumpy.
While sarcoidosis can affect anyone, it’s more common in Black people than in white people. It also affects females slightly more than males. Most cases are diagnosed between the ages of 25 and 40.
While you can’t inherit sarcoidosis, you’re at a higher risk of developing it if you have a first-degree biological relative (parent, child or sibling) who has it.
Sarcoidosis is considered a rare disease. There are usually fewer than 200,000 cases of sarcoidosis at any given time in the U.S.
The symptoms of sarcoidosis depend on where in your body granulomas form. Most people with sarcoidosis have lung symptoms, but you can have symptoms in your skin, eyes, joints and almost anywhere else in your body. You may also have general feelings of being unwell or no symptoms at all.
Advertisement
Pulmonary (lung) sarcoidosis is sometimes described in stages called the Siltzbach classification system.
It’s important to know that these stages aren’t necessarily an indicator of severity. You’re not expected to move through each stage. They’re based on your lungs’ appearance on a chest X-ray and mostly describe where the granulomas are located.
Someone with sarcoidosis can move between stages or have granulomas disappear completely. The only stage that’s irreversible is stage four, which is permanent lung damage.
Research suggests that a combination of genetics and environmental factors cause sarcoidosis, but its exact cause is unknown. We think certain people are more likely to have their immune system overreact to certain triggers (antigens), like bacteria and viruses. Despite the immune system’s involvement, sarcoidosis isn’t considered an autoimmune disorder.
Since we don’t know for sure which combination of genes and triggers causes sarcoidosis, it’s impossible to predict who will get it.
Löfgren syndrome is a sudden onset of sarcoidosis defined by a group of symptoms affecting several parts of your body:
Löfgren syndrome usually resolves in six months to two years.
Sarcoidosis is usually diagnosed with a combination of a physical exam, imaging (such as a chest X-ray) and biopsy of suspected granulomas. Because sarcoidosis can look like other conditions, your healthcare provider may perform additional tests to rule out other illnesses.
Advertisement
Imaging tests and biopsies are the most common ways to diagnose sarcoidosis, but your healthcare provider may order others based on your signs and symptoms.
More involved procedures can examine tissue from your lungs using small tubes, cameras and biopsy equipment passed through your nose, your throat or an incision (small cut). These include:
Other tests for sarcoidosis include:
Advertisement
Treatment for sarcoidosis is usually to manage symptoms and prevent organ damage. Since granulomas are areas of inflammation caused by immune cells, sarcoidosis is usually treated with medications that modify or suppress your immune system. Treatment depends on where granulomas are in your body.
There’s no specific cure for sarcoidosis, though it often goes away on its own. If symptoms aren’t bothersome or life-threatening, sarcoidosis sometimes doesn’t need to be treated immediately. You and your healthcare provider will monitor your symptoms instead.
Medications to treat sarcoidosis aim to reduce inflammation by modifying or suppressing your immune system. Some commonly used medications in sarcoidosis include:
Advertisement
Corticosteroids can put you at increased risk of getting sick with an infectious disease and can cause a number of side effects, including:
For this reason, healthcare providers only recommend using medications to treat sarcoidosis if the benefits outweigh the risks.
It can take anywhere from a few weeks to a few months for you to notice symptom improvement after starting treatment for sarcoidosis. Your healthcare provider will monitor you and may perform tests again to see if the treatment is working.
Some research suggests that certain diets reduce inflammation in the body. Eating plant-based foods (like fruits and vegetables), limiting meat and cheese, and avoiding sugar and carbohydrates (like breads) may help improve your sarcoidosis symptoms. Ask your healthcare provider before starting a new diet.
The severity of sarcoidosis is different from person to person. For most people, it’s a temporary condition that goes away on its own or with treatment. For some, it’s a chronic illness that causes permanent damage.
About two-thirds of people diagnosed with sarcoidosis will eventually be disease-free (sarcoidosis will go into remission) in two to three years. Löfgren syndrome has a particularly good prognosis, with most cases resolving in six months to two years.
Most people who still have sarcoidosis after three years are likely to have chronic disease. Only about 10% to 20% of those with chronic sarcoidosis will have permanent organ damage. The most common complication of sarcoidosis in the U.S. is lung scarring.
Most people with sarcoidosis can expect to live as long as someone without sarcoidosis. A small percentage (1% to 5%) of sarcoidosis cases are fatal.
Since we don’t know for sure what causes sarcoidosis, there’s no way to prevent it or reduce your risk of getting it. Taking medications as prescribed by your healthcare provider will reduce your risk of organ damage that granulomas can cause.
The best way to take care of yourself while living with sarcoidosis is to follow the recommendations of your healthcare provider. Monitor your symptoms for changes and take any medications as directed.
You should call or make an appointment with your healthcare provider if you have new or bothersome symptoms, or if you’re receiving treatment and experiencing worrisome side effects.
It might be helpful to ask your healthcare provider:
Sarcoidosis is a rare condition with many possible symptoms. Many cases resolve on their own or with treatment, but chronic sarcoidosis can be managed with medications and careful monitoring. It’s important to note that in some cases, it may be beneficial to monitor symptoms without treatment. You and your healthcare provider can make a plan that works for your specific case.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Sarcoidosis can take you by surprise. Cleveland Clinic has a team of sarcoidosis experts who offer personalized treatment options that match your needs.
