Postherpetic neuralgia (PHN) causes persistent pain after you have shingles. “Neuralgia” means “nerve pain.” You’ll typically have pain in the same areas where you had a shingles rash. It’s the most common complication of shingles, but not everyone develops it. Several medications and other therapies can help you manage PHN pain.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
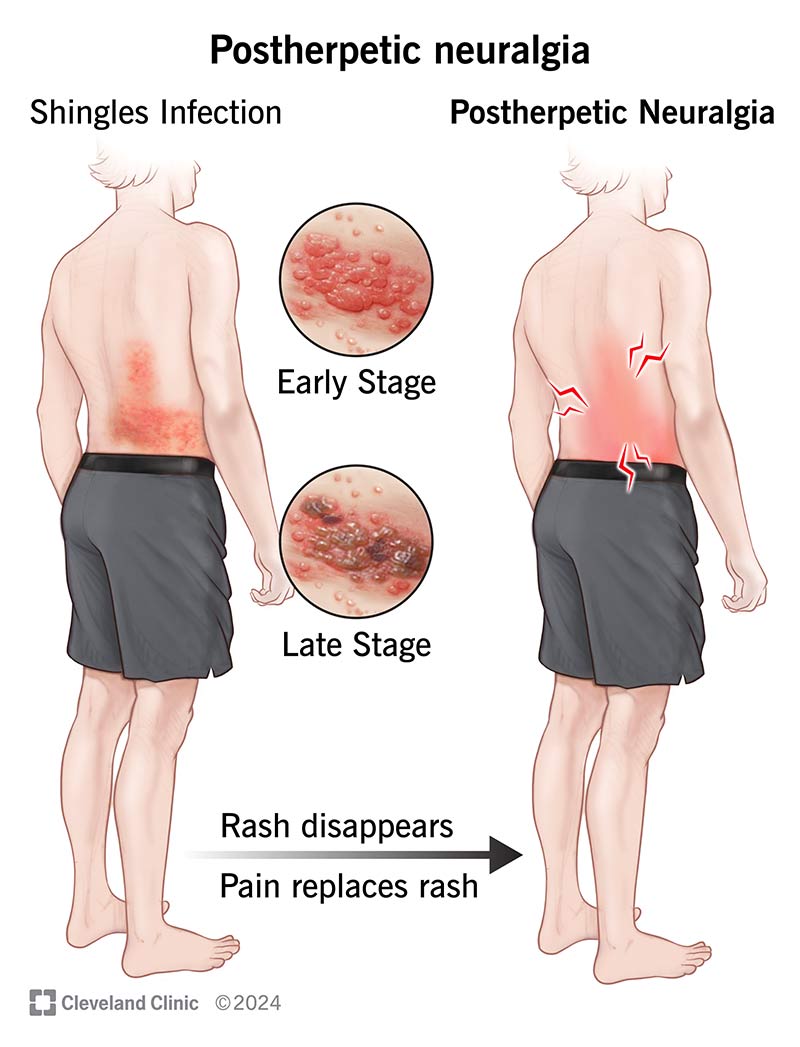
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/12093-postherpetic-neuralgia)
Postherpetic neuralgia (PHN) is a complication of the shingles infection. It causes persistent pain where you had a rash and blisters. The pain stays after the rash and blisters go away. The same virus that causes chickenpox can wake up later in life and cause shingles (also referred to as herpes zoster).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
PHN is the most common complication of shingles. About 1 to 2 out of every 10 people who get shingles also develop this condition.
Pain can wear you down physically, mentally and emotionally. Talking with your provider is an important first step. Together, you can create a plan to help manage the pain and improve how you feel each day.
Symptoms may start while you have a shingles rash or after the rash goes away. This could be a few weeks to months later. Symptoms could include:
The pain can feel different from person to person.
PHN happens when shingles damages your nerve fibers. These damaged nerves send stronger pain signals to your brain than they should. This causes ongoing pain. Doctors still don’t know exactly why some people develop this condition after shingles while others don’t.
The same virus that causes chickenpox (varicella-zoster virus) also causes shingles. After you have chickenpox, the virus stays in your body. It stays “asleep” for many years. If the virus becomes active again, it causes shingles.
Advertisement
You may be at higher risk of developing PHN if you:
Living with long-term pain can affect many parts of your life and health, like:
If pain is making your daily life difficult, it’s important to ask for help. And you may want to talk to a mental health professional for emotional support resources.
Most of the time, doctors can tell if you have PHN by:
If you had shingles without a rash or a rare type that affects your throat, your provider may order lab tests or imaging tests to be sure.
If you have PHN, your healthcare provider will likely start by prescribing one of these medications:
Each of these medications has different side effects. They can also interact with other medications you take. Your provider will carefully review the possible side effects and risks with you.
It may take time to find a treatment that relieves symptoms. You may need to try more than one medication, or your provider may prescribe several medications at the same time. Contact your provider if your symptoms don’t improve. Take all of your medications exactly as prescribed.
For long-lasting and difficult-to-treat cases, your provider may recommend more invasive treatments for pain management, like:
While there isn’t a cure, there are treatments that can help lower how much pain you feel. Managing pain may take time. It could involve trying different treatments to find what works best for you. Some may help more than others. You’ll likely need to keep working with your provider to adjust your care as needed.
Coping with PHN takes patience. Taking care of both your body and mind can make a big difference. Talking with a mental health professional may also help you manage the emotional side of living with pain.
Advertisement
How long PHN lasts can be different for each person. For many, the pain lasts for months or even years. In some cases, the pain may never go away completely. But treatment options can help you manage it.
The best way to prevent PHN is by getting the shingles vaccine. The vaccine reduces your chances of getting shingles and the long-lasting nerve pain that can come with it. Adults usually get the vaccine in two doses, a few months apart.
There’s also a chickenpox vaccine. If you or your children have never had chickenpox, getting this vaccine may help prevent the virus from entering your body. If you never get chickenpox, you can’t get shingles or PHN later in life.
You may be living with postherpetic neuralgia (PHN), but at times, it might feel like you’re just getting through the days with pain. The symptoms can wear you down. You might feel too tired to run errands, find it hard to focus at work or skip time with friends because you’re not feeling your best.
Even though the pain is real, it doesn’t have to take over your life. A healthcare provider can help you manage it. There’s no one-size-fits-all treatment for PHN. It may take time to find what works best. But getting the right care may help you feel more like yourself again.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Need care fast? Cleveland Clinic’s Express Care and Urgent Care locations treat everything from sprains to sinus infections — no appointment needed.
