Lupus is an autoimmune disease that makes your immune system damage organs and tissue throughout your body. It causes inflammation that can affect your skin, joints, blood and organs like your kidneys, lungs and heart. A healthcare provider will help you find medications to manage symptoms and reduce how often you experience flare-ups.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Lupus is an autoimmune disease that causes inflammation throughout your body. If you have lupus, your immune system damages your body instead of protecting it.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Lupus can damage your:
Visit a healthcare provider if you notice new pain, rashes or changes to your skin, hair or eyes.
Healthcare providers sometimes call lupus systemic lupus erythematosus (SLE). It’s the most common type of lupus. It means you have lupus throughout your body. Other types include:
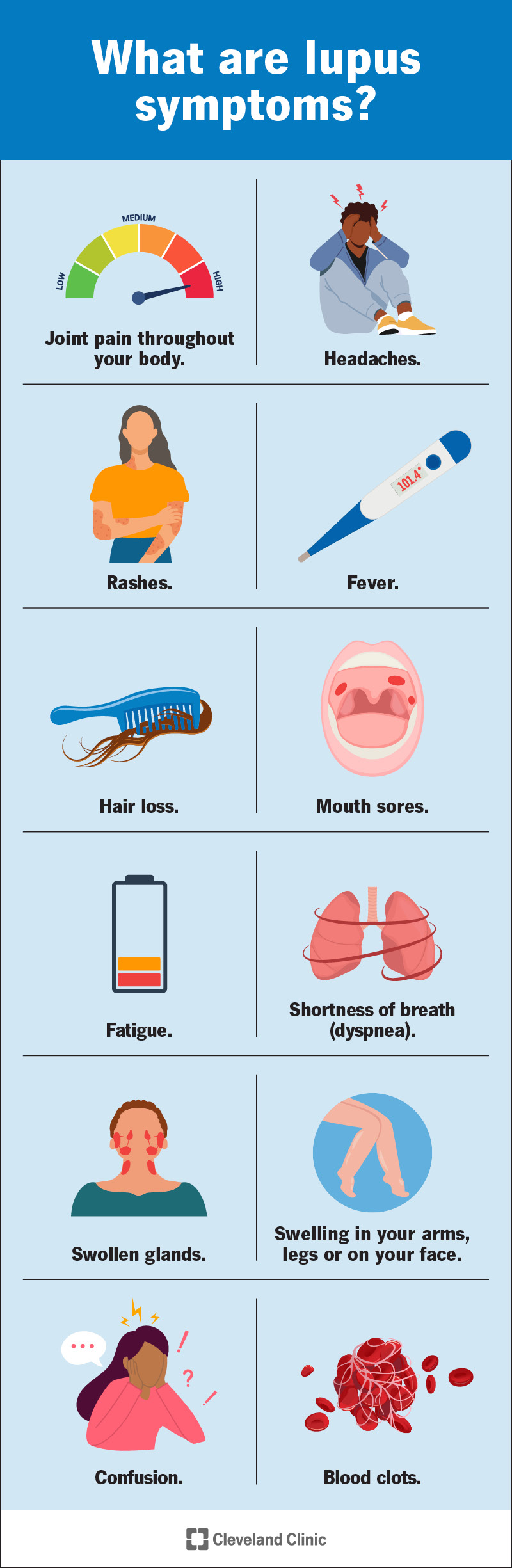
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/4875-lupus-infographic)
Where you have symptoms depends on which organs or systems lupus affects. Everyone experiences a different combination and severity of symptoms.
The most common symptoms include:
Advertisement
Lupus symptoms usually come and go in waves called flare-ups. During a flare-up, the symptoms can be severe enough to affect your daily routine. In between flares, you might have periods with mild or no symptoms. This is called being in remission.
Symptoms usually develop slowly. You might notice one or two signs of lupus at first. Then, you might experience more or different symptoms later on.
Lupus sometimes leads to other health conditions. The damage to your organs and tissue can add up over time and lead to new or different issues. Some lupus complications can include:
Experts don’t know for sure what causes lupus. Certain factors about your health or where you live may trigger lupus, including:
Anyone can develop lupus. You have a higher risk if one or both of your biological parents have it. Your lupus risk will also be higher if you’re:
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_k80l25xx/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Learn what lupus is and how it’s diagnosed.
A healthcare provider will diagnose lupus with a physical exam and some tests. They’ll ask about the symptoms you’re experiencing. Tell your provider when you first noticed symptoms or changes in your body. Your provider will ask about your medical history, including conditions you have now and how you’re managing them.
Lupus can be tricky to diagnose because it can affect so many parts of your body. And it causes lots of different symptoms. Even small changes or issues that seem unusual can be key. Don’t be afraid to tell your provider about anything you’ve felt or sensed. You know your body better than anyone.
There’s not one test that can confirm a lupus diagnosis. Diagnosing it is usually part of a differential diagnosis. This means your provider will probably use a few tests to determine the cause of your symptoms. They’ll rule out other, more common conditions before diagnosing lupus. You might need:
Advertisement
Your healthcare provider will suggest treatments that manage the symptoms. The goal is minimizing damage to your organs and how much lupus affects your day-to-day life. You’ll probably need a combination of medications. They can reduce how often you experience flare-ups and lessen how severe symptoms are when you have one. Some of the most common SLE medications include:
You might need other medications or treatments to manage specific lupus symptoms or other health conditions it’s causing. For example, you may need treatment for anemia, high blood pressure or osteoporosis if lupus causes those issues.
Advertisement
You might be able to prevent and reduce lupus flare-ups by avoiding activities that trigger symptoms, including:
Visit a healthcare provider as soon as you notice any new or changing symptoms. Even small shifts in what you’re feeling and experiencing can be important.
Advertisement
Talk to your provider if it feels like your treatments aren’t working as well as they used to. Also, tell your provider if you’re having flare-ups more often, or if they’re causing more severe symptoms. Your provider can help you adjust your treatments as needed.
Go to the emergency room or call 911 (or your local emergency services number) if you’re experiencing any of the following symptoms:
Lupus is a lifelong (chronic) condition. You should expect to manage it for the rest of your life.
It can be unpredictable. And the way it impacts you can change over time. You’ll need to visit your healthcare provider regularly so they can track changes in your body.
You’ll probably work with a team of providers as you learn to live with lupus. Your primary care provider will suggest specialists who can help with specific issues or symptoms. You’ll probably need to visit a rheumatologist. This is a healthcare provider who specializes in diagnosing and treating autoimmune diseases. Which specialists you need to visit depends on the symptoms you have and how they affect your body.
There’s currently no cure for lupus. Your healthcare provider will help you find a combination of treatments to manage the symptoms. You may be able to enter remission once you find treatments that work for you. Even if you have long periods of time with no symptoms or flare-ups, there’s always a chance lupus will come back. Your care team will help you set goals and expectations based on your unique circumstances.
Lupus can be a frustrating, tiring condition. Pain, inflammation and irritation throughout your body can be exhausting. But don’t forget to appreciate yourself. Living with a chronic condition is hard work, and you deserve credit for managing the symptoms every day. Ask your provider about mental health resources and support groups if you think talking to someone about how you’re feeling could help you.
Don’t be afraid to talk to your provider and ask any questions you have. Even small changes in your health can be a sign that lupus is affecting you differently. Remember, you’re the best judge of when something isn’t quite right in your body.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Knowing your body’s immune system is battling itself can be stressful. Cleveland Clinic’s lupus experts are here to treat and manage your disease for the long haul.
