The sphincter of Oddi is a muscle that opens and closes to allow bile and pancreatic juice to flow into your small intestine. In sphincter of Oddi dysfunction, your sphincter muscle doesn’t open when it should, which causes a backup of digestive juices and severe pain in your abdomen. Healthcare providers treat this condition with medications or a procedure called a sphincterotomy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
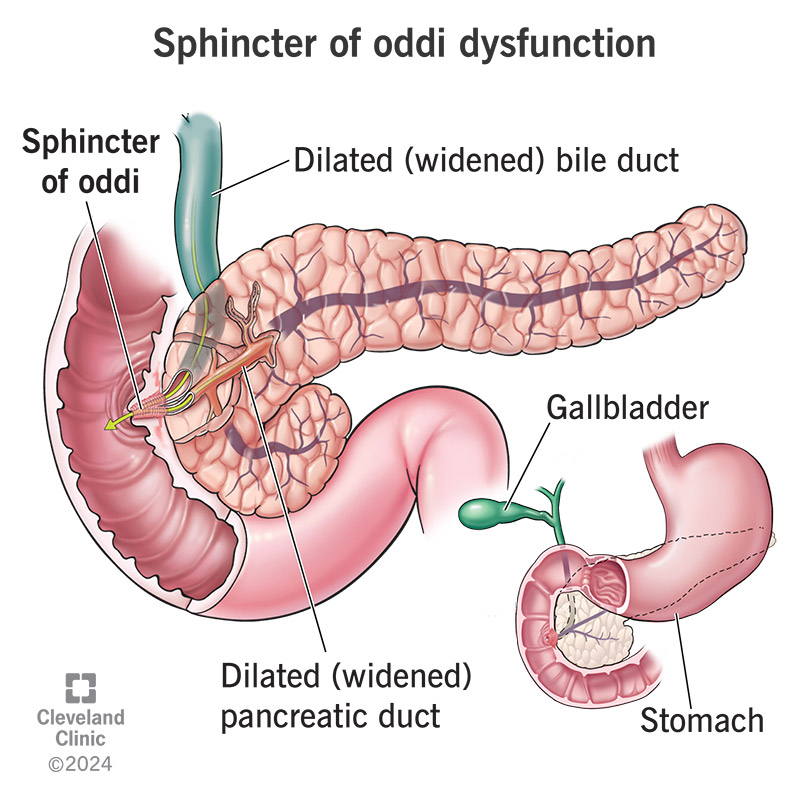
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/14516-sphincter-of-oddi-dysfunction.jpg)
Sphincter of Oddi dysfunction occurs when a muscle called the sphincter of Oddi doesn’t open when it should to allow the flow of digestive juices. This causes a backup of digestive juices, leading to severe abdominal (belly) pain.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Digestion is a complex process where your body transforms food into energy. Your liver, pancreas and the sphincter of Oddi all play important roles. Your liver produces a chemical called bile that’s stored in your gallbladder. Your pancreas produces enzymes. These digestive juices flow into your small intestine. A muscle called the sphincter of Oddi controls their flow.
When it’s working properly, the sphincter of Oddi opens to allow bile and pancreatic juice to flow through. Then, it closes again. However, with sphincter of Oddi dysfunction, the sphincter muscle doesn’t open as it should. The digestive juices get trapped behind the sphincter of Oddi and cause symptoms similar to what people experience with gallbladder pain.
People who’ve had their gallbladders removed are most likely to develop sphincter of Oddi dysfunction. The procedure to remove the gallbladder is called cholecystectomy, and sphincter of Oddi dysfunction is often called “post-cholecystectomy syndrome.”
There are two basic types of sphincter of Oddi dysfunction:
Advertisement
There are also three categories of sphincter of Oddi dysfunction:
Researchers estimate that about 20% of people who experience ongoing pain after gallbladder removal surgery have sphincter of Oddi dysfunction.
It’s not life-threatening, and it usually doesn’t cause complications. Still, the pain it causes can interfere with your quality of life. Treatment can provide needed symptom relief that improves your overall health and well-being.
The most common symptom is abdominal pain that’s similar to gallbladder pain. It may feel like a stabbing pain that starts on your upper right side. Sometimes, it radiates to your right shoulder or back. Usually, the pain lasts for 30 minutes to an hour but then resolves until the next symptom flare-up.
The symptoms of sphincter of Oddi dysfunction include:
These symptoms can come and go and can be mild one time but severe the next.
Researchers haven’t identified a single cause. Sphincter of Oddi dysfunction manifests in different ways, which means there may be several contributing factors. Sometimes, sphincter of Oddi dysfunction is related to issues like scarring and inflammation that prevent the free flow of pancreatic juice or bile into your small intestine. Other times, there’s a problem with how the sphincter opens and closes.
You’re more likely to develop sphincter of Oddi dysfunction if you’re a female between 20 to 50 years old who’s recently had gallbladder surgery. Still, several conditions and procedures can increase your risk of developing this condition.
Risk factors include:
Advertisement
Left untreated, sphincter of Oddi dysfunction can lead to:
If your healthcare provider suspects you have sphincter of Oddi dysfunction, they’ll first check to see if another condition is causing your abdominal pain. They’ll rule out peptic ulcer disease or stones in the ducts that carry bile from your liver (choledocholithiasis). It’s important to make sure people with abdominal pain don’t have serious conditions like pancreatic cancer or bile duct cancer.
In some cases, even heart conditions such as angina (chest pain) or ischemia (the heart doesn’t get enough blood) can cause pain that seems to be coming from your abdomen.
Your healthcare provider will perform blood tests to check for elevated liver and pancreatic enzyme levels. You may need abdominal imaging or scope tests to check for any abnormalities in your sphincter or ducts, including:
Advertisement
Some centers perform a test called endoscopic retrograde cholangiopancreatography (ERCP) with manometry. For this test, a healthcare provider places a small plastic tube into the pancreas duct or bile duct near the sphincter of Oddi to measure how well it’s contracting and expanding. Other centers perform ERCP without manometry, but with a plan to perform a sphincterotomy (a type of treatment) in people who likely have sphincter of Oddi dysfunction.
This test isn’t without risk. Up to 30% of people who get this procedure develop pancreatitis. Providers are increasingly using new, less invasive technologies to diagnose sphincter of Oddi dysfunction. These technologies include hepatobiliary scintigraphy. This test can show how digestive fluids flow into your small intestine and at what rates.
Scientists continue to research the safest and most reliable tools to diagnose sphincter of Oddi dysfunction.
If the pain isn’t too severe (especially if you have hard-to-diagnose category III disease), your healthcare provider will prescribe non-opioid pain medications or medicines to relieve spasms.
If the pain is severe and you have category I or II disease, your provider may refer you for an ERCP with sphincterotomy. You’ll either be sedated or put to sleep under general anesthesia for this procedure. A surgeon will pass a thin instrument into the area of your small intestine where the sphincter of Oddi is and cut the muscle. The surgeon will also ensure that there aren’t any stones in your bile ducts.
Advertisement
Studies show that sphincterotomy isn’t effective for treating category III sphincter of Oddi dysfunction.
In most cases, sphincterotomy can help relieve the pain and other symptoms of sphincter of Oddi dysfunction in people with category I or II sphincter of Oddi dysfunction. However, your provider will likely try this procedure only if other treatments don’t help.
Sphincterotomy is a complex procedure that has a fairly high risk of complications. About 10% to 15% of patients have complications such as inflammation of the pancreas. This inflammation is usually mild but can be severe and even life-threatening. In some cases, the complications are severe and can require a long stay in the hospital.
Treatment doesn’t completely resolve sphincter of Oddi dysfunction symptoms, but it can provide better pain management and greatly improve your quality of life.
Sphincterotomy improves symptoms in up to 90% of people with category I disease and up to 70% with category II disease. Most people with category III sphincter of Oddi dysfunction get pain relief by taking pain medicines.
Questions to ask your provider include:
Sphincter of Oddi dysfunction is a frustrating diagnosis, especially if it involves ongoing gallbladder pain even after removing your gallbladder. Medications often relieve symptoms, so you don’t have to have additional surgery, like a sphincterotomy. But if the medications aren’t helping enough, this surgery relieves symptoms for most people with this condition.
Follow your healthcare provider’s guidance on the best treatment options based on your unique condition. Weigh the pros and cons of treatments and ask about follow-up care should you develop a complication afterward, like pancreatitis.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have issues with your digestive system, you need a team of experts you can trust. Our gastroenterology specialists at Cleveland Clinic can help.
