Mixed connective tissue disease (MCTD) is a rare inflammatory autoimmune disorder that has symptoms and signs of several other disorders, including lupus, scleroderma and polymyositis. Many people with MCTD also have rheumatoid arthritis and/or Sjögren’s syndrome. Treatment varies depending on your symptoms and severity of the condition.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
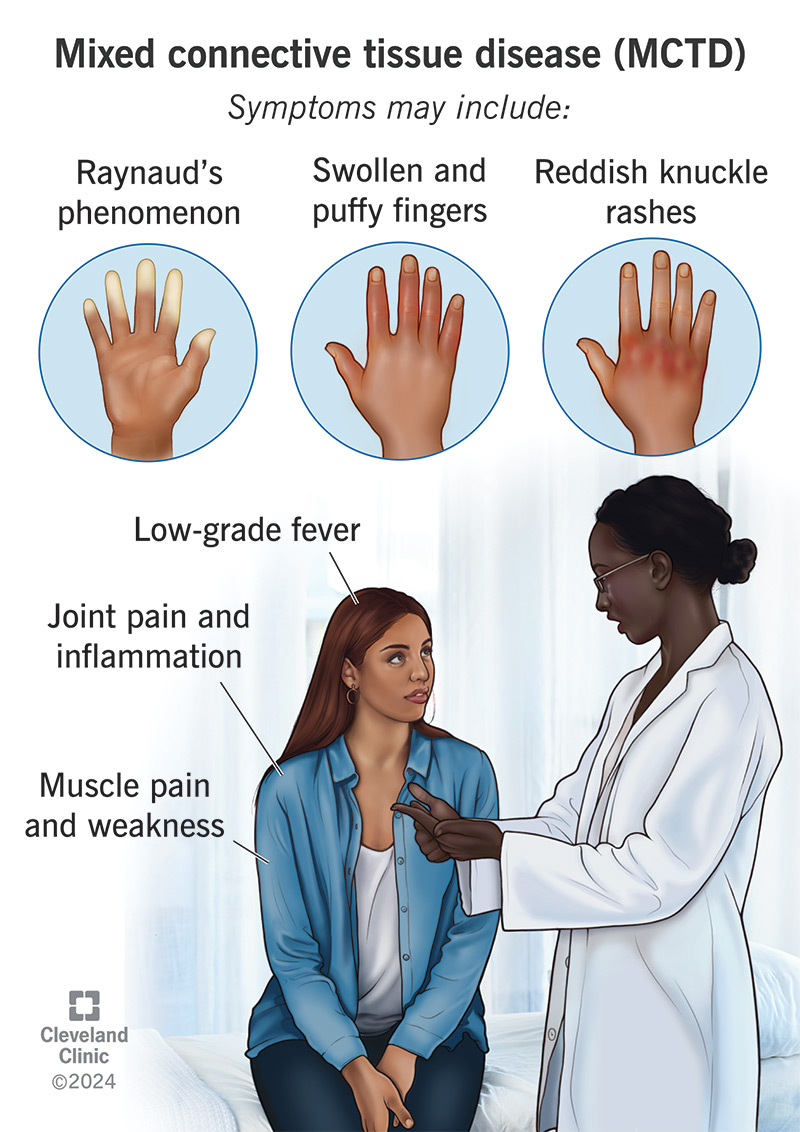
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/mixed-connective-tissue-disease)
Mixed connective tissue disease (MCTD) is a rare autoimmune disorder. An autoimmune disorder is one in which your immune system mistakenly views your body’s own tissues as “invaders” and attacks them. Mixed connective tissue disease has features of three other connective tissue diseases:
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Some people also show signs of dermatomyositis, rheumatoid arthritis or Sjögren’s syndrome. About 25% of people with a connective tissue disease develop another connective tissue disease over the course of several years. This is why MCTD is known as an “overlap syndrome.”
Symptoms of different connective tissue disorders typically occur over time, not all at once. MCTD symptoms may include:
During an MCTD flare-up, you may feel severe joint and muscle pain. Your joints may inflame and swell, causing intense pain and stiffness. This is similar to what rheumatoid arthritis feels like.
Your fingers, hands and sometimes toes may suddenly feel numb and tingly. They may become pale and then purple or blue in response to the cold or stress. These are symptoms of Raynaud’s phenomenon.
Advertisement
Researchers don’t know what triggers mixed connective tissue disease. It’s not directly inherited, although some research shows that the disease may occur more often in people with a biological family history of connective tissue diseases. Exposure to certain viruses, chemicals or materials, like polyvinyl chloride and silica, are other possible causes.
MCTD occurs most often in females in their 20s and 30s. But people of all ages, including children, can develop the disease.
Mixed connective tissue disease (MCTD) can lead to severe complications, including:
MCTD can be difficult for healthcare providers to diagnose because the three conditions (lupus, scleroderma and polymyositis) that combine and cause it usually don’t happen at the same time. Because they occur one after the other over a long period of time, it may take several years before a provider can make an accurate diagnosis of MCTD. You’ll likely work with a specialist called a rheumatologist in the diagnosis of MCTD.
There are four features that point to MCTD rather than another connective tissue disorder:
Treatment for MCTD depends on which organs are affected, your symptoms and how severe your condition is. Some people may need treatment only during flare-ups, while others may require constant care. There’s no cure for the disease, but medication can help you manage your symptoms. MCTD medications may include:
Advertisement
If you have mixed connective tissue disease, you’ll likely need prescription medications to manage your symptoms. But you can also take steps to manage the disease on your own by:
Long-term corticosteroid use can lead to side effects like:
You must see your healthcare provider on a regular basis to monitor and control these possible effects.
Women with MCTD who are thinking of becoming pregnant should talk to their provider first. Pregnancy can increase flare-ups of the disease, and babies born to women with MCTD may have low birth weight.
Advertisement
People who have a long-term, incurable condition like MCTD should develop ways of dealing with their disease. This includes:
You should see a healthcare provider if you develop any of the signs or symptoms of a connective tissue disease, especially if they interfere with your daily routine. Any new muscle or joint pain, puffy fingers or signs of Raynaud’s phenomenon should warrant a call to a provider to see what’s going on.
If you’re going to see your provider about a possible mixed connective tissue disease diagnosis, you may want to ask the following questions:
As MCTD is composed of a number of connective tissue disorders, there are many different possible outcomes, depending on:
Advertisement
With proper treatment, 80% of people survive at least 10 years after diagnosis. But your healthcare provider is the best source of information for your specific case.
If you’ve been feeling unwell with joint or muscle pain and puffy or even numb fingers — a mix of symptoms — you may have a condition known as mixed connective tissue disease (MCTD). This condition is an overlap of several different connective tissue diseases. It can be uncomfortable or downright debilitating during a bad flare-up. While there’s no cure for MCTD, your healthcare provider can help you find ways to manage your symptoms so you can get back to living your life.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic provides accurate diagnoses and personalized treatments for all types of autoimmune disorders, including lupus, MS and rheumatoid arthritis.
