Nasal polyps are soft, painless, noncancerous growths that can form in the lining of your nose or sinuses. They happen most often in people with asthma, allergies, repeat infections or nasal inflammation. Medication and outpatient surgery can shrink nasal polyps and relieve symptoms.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
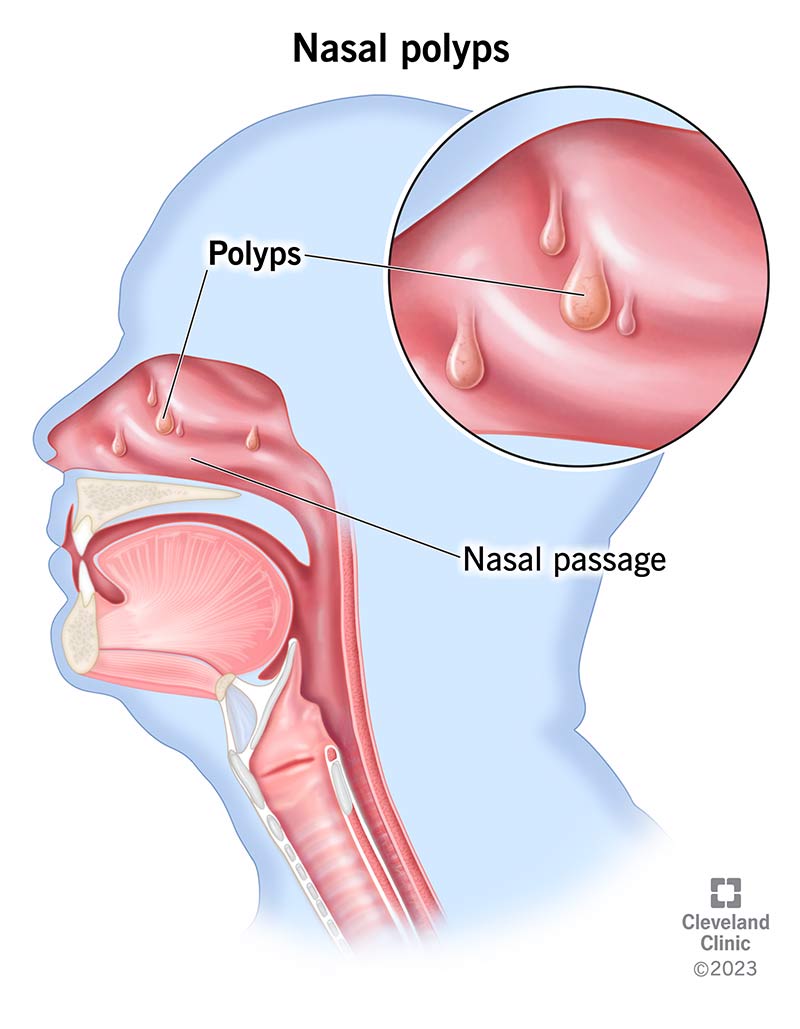
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/nasal-polyps)
Nasal polyps are painless and benign (noncancerous) growths. They form in the mucosa (thin, soft tissue) that lines your nasal and sinus passages. They usually appear on both sides of your nose. Nasal polyps can get irritated and swollen, making it hard for you to breathe through your nose.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Small polyps are teardrop-shaped. But as they grow larger, they often resemble peeled grapes that are pink, yellow or gray.
Nasal polyps affect up to 40% of the general population. Anyone can get them. But they’re twice as common in men. Many people get them in their 30s or 40s. But the overall risk increases with age.
Nasal polyposis is another name for nasal polyps.
Small polyps in your nose might not cause symptoms at all. But if they start to grow, you could develop:
When polyps grow large enough, they can block your nasal passages and sinuses, leading to:
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_iwgm017l/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Nasal polyps are soft, painless, noncancerous growths that can form in the lining of your nose or sinuses.
Healthcare providers know that inflammation causes nasal polyps. But they don’t know why some people go on to develop polyps because of inflammation while others don’t.
Chronic sinusitis — from allergies, infection or asthma — seems to be the most common reason polyps appear. Chronic sinusitis refers to nasal and sinus inflammation that’s lasted three months or longer. But several risk factors could contribute to the development of nasal polyps.
Advertisement
A risk factor is something that increases your chance of getting a certain condition. Nasal polyp risk factors include existing health conditions like:
Genetics may also play a role in the development of nasal polyps. For instance, certain gene mutations (changes) may impact how your nasal tissues react to inflammation.
Ongoing sinus infections associated with nasal polyps can result in rare but serious complications like:
To diagnose nasal polyps, a healthcare provider will start with a physical examination. During this appointment, they may:
If your healthcare provider needs more information, they may order one of these imaging tests to help them determine the size and location of each polyp:
Your provider may also recommend allergy testing. This can help them identify allergens that lead to nasal inflammation and polyps.
Nasal polyp treatment depends on the severity of your condition. Medication and surgery are the two main approaches.
Even with surgical removal, nasal polyps may grow back over time. Your healthcare provider will talk to you about the likelihood of recurrence (return) and how you can manage it.
Medication usually doesn’t get rid of nasal polyps, but it can ease symptoms. Common treatments include:
Your healthcare provider also may prescribe antibiotics if you have an infection.
If medication doesn’t work — or if you have large polyps — you may need sinus surgery to remove them. Your provider may use nasal endoscopy to do one of these minimally invasive procedures:
Advertisement
All these procedures are minimally invasive. That means your surgeon does everything through your nostrils. So, you won’t have visible incisions or sutures.
Treatment can help you get rid of nasal polyps and make it easier for you to breathe through your nose. But unfortunately, polyps can come back after treatment. Some people need to stay on steroid medications or have repeat surgery to manage them.
People with loss of taste (ageusia) and loss of smell (anosmia) may not see a total improvement of symptoms after treatment. Ask your healthcare provider what you should expect in your case.
It’s not always possible to prevent nasal polyps. But here are a few things you can do to reduce your risk:
Schedule an appointment with your healthcare provider if you have nasal polyp symptoms that last longer than 10 days.
Additionally, let your provider know if you notice a single growth on one side of your nose. This could be a nasal or paranasal tumor rather than a polyp.
Advertisement
Consider asking your healthcare provider:
In some cases, nasal polyps can shrink on their own over time. But they rarely go away. People who have severe symptoms will likely need treatment.
You usually can’t see nasal polyps by looking up your own nose. But if they grow large enough, a provider might be able to see them if they look up your nose with a nasoscope (lighted tool).
Trauma or blowing your nose really hard can cause nasal polyps to swell or become dislodged. Nasal steroid sprays may help reduce inflammation and help the polyps return to their original position.
You should never — under any circumstances — try to remove nasal polyps yourself. Doing so can lead to injury, excessive bleeding and infection.
Nasal polyps can make your nose feel stuffy all the time. Left untreated, they can interfere with your breathing and ultimately lead to bone and tissue damage. If you develop nasal polyp symptoms, tell your healthcare provider right away. They can find a treatment option that works for your situation.
Advertisement
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Nasal polys can be stubborn. Cleveland Clinic’s experts can help treat your nasal polyps and relieve symptoms that get in the way of your life.
