
“Someone had to go first,” says Faith Rife as she reflects on her experience undergoing a novel procedure. Grappling with several heart defects, it became clear the avid gym-goer needed a new solution with her health and quality of life deteriorating.
“Just walking up a few steps, I noticed I’d be huffing and puffing,” says Faith. “When working out, I’d start turning blue.”
Faith was born with multiple heart abnormalities, including a double outlet right ventricle and a rare rotational anomaly called criss-cross heart. Double outlet right ventricle means she was born with both of her heart’s main arteries connecting to her right ventricle, whereas normally, one artery should connect to the left ventricle as well. The criss-cross heart refers to her atrioventricular valves being positioned in an abnormal crossed pattern, with her two ventricles positioned one above the other – rather than being side by side, like they typically should. She also had a ventricular septal defect, which is a hole in the wall between her heart’s two lower chambers. All of this meant she wouldn’t be able to effectively pump blood, eventually leading to serious complications like heart failure without treatment.
Through prenatal imaging, Faith’s mom, Julia Kable, says they were aware Faith had heart defects before she was born. Faith was delivered in a pediatric intensive care unit at a local hospital near where they lived in Columbus, Ohio.
“They had a whole team there waiting for her – ready to respond. But she came out fat, sassy and pink. You would not have known there was a thing wrong with her,” laughs Julia.
Faith continued thriving for her first week until she couldn’t eat and started losing weight. When she was a little over 3 weeks old, Faith’s doctor said she needed surgery quickly.

Although they were prepared for the worst, Faith’s mom Julia says you couldn’t tell anything was wrong with Faith shortly after she was born. She wouldn’t go on to have her first surgery until she was a few weeks old. (Courtesy: Julia Kable)
“They decided this was urgent after she had lost two pounds. And because of the complexity of the surgery, our pediatric cardiologist wanted us to go to Cleveland Clinic Children’s,” says Julia.
Once at Cleveland Clinic, doctors opted to perform what’s called a pulmonary artery banding. With Faith’s heart pumping too much blood to her lungs, this procedure would reduce that blood flow, helping to prevent lung damage and manage her heart’s workload. It’s meant to be a temporary fix until further surgeries can be done since the band becomes too tight as the child grows.
“After this, Faith bounced back quickly, and we were home from the hospital in five days. She was growing and thriving up until she was a little over a year old. That’s when we started having trouble again,” says Julia.
With the pulmonary artery banding no longer effective, Faith underwent the Glenn procedure. The procedure helps those with only one working ventricle by sending blood directly to the lungs and bypassing problematic areas of the heart. It’s often performed as part of a series of surgeries, with the Fontan procedure being the last.

Faith underwent the majority of her surgeries during early childhood. (Courtesy: Julia Kable)
“Again, she tolerated this pretty well and recovered quickly. We took her home, and life was good until she was about 4 years old,” says Julia. That’s when Faith started developing veno-venous collaterals, which are abnormal blood vessels the body creates to bypass blood flow blockages. These can burst or bleed, leading to different issues.
“The first memory I have of something being wrong came when I was playing with my brother, and then, all of a sudden, I started coughing up blood,” says Faith. Due to this complication, doctors proceeded with the Fontan procedure.
Following these surgeries, Faith says it didn’t really occur to her growing up that her heart was different than anyone else’s. Aside from sometimes struggling to keep up with her classmates, she says it didn’t impact her much.
“If I wanted to try something the other kids were doing, my mom encouraged me to. Unless it was something that would hurt me, I tried out everything I wanted,” says Faith.

After her initial surgeries, Faith had her next procedure when she was 22 years old. (Courtesy: Julia Kable)
As her care team closely monitored her, Faith says she felt well overall for years. She found her passion for working out and even took on martial arts and boxing. Over time, however, she developed some concerning symptoms.
“At the gym, I was noticing my lips and fingers turning blue. At home, I’d walk up one flight of stairs and need to sit down because I’d be so exhausted. I was constantly fatigued,” says Faith, who started experiencing these more severe symptoms in high school.
Faith says her doctors told her early on she might need another surgery down the road. That’s because the altered circulation in the body from the Fontan can lead to complications over time, including with organ function. In Faith’s case, testing showed her liver, lungs and kidneys were all being impacted. She also had an obstruction below the aortic valve that was progressing, causing her heart to work even harder.
“We discussed Faith’s options with her, and one of them involved a novel division of her heart to return it to a two-ventricle system. This would include a valve implantation,” says Hani Najm, MD, a pediatric and congenital heart surgeon at Cleveland Clinic Children’s. “The timing was right because she was well enough to withstand a major surgery and keep her own heart. Had we waited, she might ultimately have needed a heart and lung transplant.”

The 3D-printed model of Faith’s heart, which played an important role in planning for surgery. (Courtesy: Cleveland Clinic)
As part of Faith’s workup for this novel approach to a biventricular conversion, Dr. Najm and his team used advanced imaging to create a 3D-printed model of her heart. This model helped Dr. Najm determine the procedure would be possible and was crucial for surgical planning.
“Using the model and other imaging, I decided I can actually separate her ventricles, using the left ventricle to pump blood to the body, and then repurpose the remaining portion of the right ventricle to pump blood to the lungs,” says Dr. Najm. “The 3D-printed model is an exact replica of the heart. So, when it’s time for surgery, I have already seen the heart and know what I’m going to do.”
Although Dr. Najm’s unique approach to this type of biventricular conversion was novel, Faith decided to move forward with it. In fact, she says she didn’t have any hesitation regarding the procedure.

Dr. Hani Najm and his team performed Faith’s procedure in August 2023. (Courtesy: Cleveland Clinic)
“I told my mom somebody has to go first, and I trusted Dr. Najm. He talked through everything with me and put a lot of thought, effort and care into the planning,” says Faith.
Julia adds, “When Faith was little, I always told myself I have to keep her healthy and well until technology and medicine catch up with her, so I prayed a lot. And when this surgery was first proposed, I thought this sounds exactly like what I've been praying for.”
In August 2023, at 22 years old, Faith underwent the novel procedure – performed by Dr. Najm and his team. Dr. Najm explains everything went well, but her heart took time to adjust since both of her ventricles had been pumping as a single ventricle for years. Following the procedure, she experienced diastolic dysfunction, which is a problem with diastole, the first part of your heartbeat. It occurs when the heart’s lower chambers don’t relax as they should. With this, Faith says she experienced issues with fluid building up in parts of her body and lungs.
“My feet and legs were swollen, and then my joints would start hurting,” says Faith. “My lungs were also irritated, which made it very difficult to lay down or sleep.”
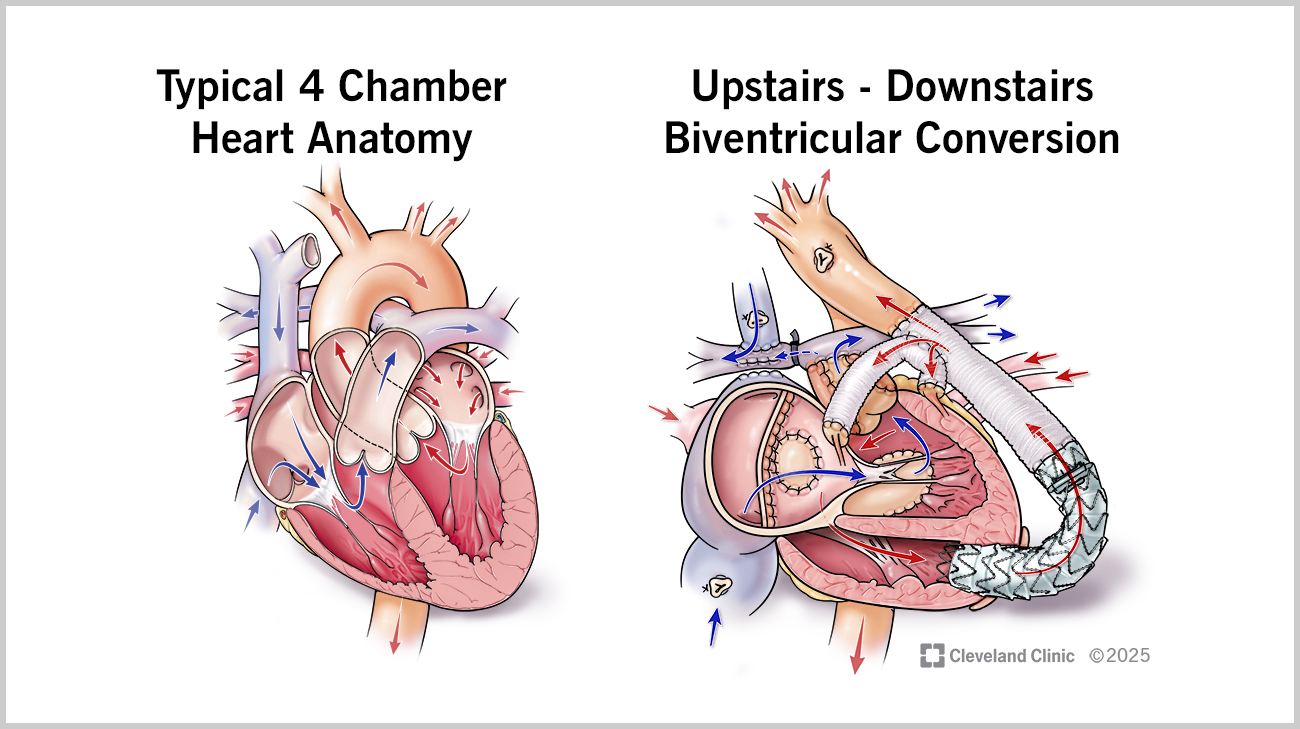
An illustration comparing a typical heart’s anatomy to what Faith’s heart looks like now after having the biventricular conversion. (Courtesy: Cleveland Clinic)
Faith’s care team worked closely with her to manage the condition, and after six long weeks in the hospital, she was able to return home. However, her recovery was just getting started. As Faith’s body continued adjusting, she needed to be on oxygen and had challenges getting her energy levels up.
“When I got home, I didn’t want to do anything. I would just sleep most of the day. I had oxygen at all times, even when I’d go out somewhere. We would even use a wheelchair for me occasionally because I’d get tired walking around,” says Faith.
During this time, Julia moved in with Faith to help take care of her. From monitoring her blood pressure to tracking her fluid intake, Julia says they followed the same protocol they had been in the hospital at home. Although it took many months for Faith to recover, she no longer requires oxygen and is returning to her normal life.
“I’ve been able to go back to the gym, and I don’t need to sit down after going up some steps. I’m feeling like myself again,” says Faith. And after taking time off for the surgery, she’s now back to work and started college classes again to be a physical therapist.

Faith at a follow-up appointment with Dr. Patcharapong Suntharos. (Courtesy: Cleveland Clinic)
After the successful surgery, Faith continues following up with her pediatric cardiologist Patcharapong Suntharos, MD, who she says has played an important part in her health journey. “My mom and I love him so much. Dr. Suntharos is always very happy and willing to explain things. He’s also very kind and empathetic when it comes to any situation,” says Faith.
As her clinical condition continues to improve, Dr. Najm doesn’t anticipate Faith will need any further surgeries at this point. He hopes her case can serve as an example for others with single ventricle defects.
“The biventricular conversion alleviated Faith’s subaortic right ventricular outlet obstruction, relieved her symptoms, improved her quality of life and avoided a future heart transplant,” says Dr. Najm. “Biventricular conversion should be considered, whenever possible, for individuals with early Fontan-related complications, who are clinically well and have no overt organ failure.”

Faith is back to enjoying the gym with her brother, Noah, and partaking in some of her favorite hobbies from gaming to crafting. (Courtesy: Faith Rife)
Although it was a challenging journey to get to where she is today, Faith says she’s thankful to have gone through with the procedure.
“I’ve always loved seeing the payoff from exercising. I’m excited to see if I can physically reach these goals I have for myself now, whereas before, I may not have been able to,” says Faith. “Being the first person to have this surgery, I wanted to share my story in case it can help someone else out there.”
Related Institutes: Heart, Vascular & Thoracic Institute (Miller Family), Cleveland Clinic Children's

