
At one point in her health journey, Sarah Minton recalls planning her own funeral because of how sick she was. Today the 42-year-old will tell you she feels like she’s 18 again. Sarah credits her remarkable progress to a second opinion that spared her from needing a double-lung transplant on top of a life-saving liver transplant.
“I knew it was going to be hard enough to have a liver transplant and felt I wouldn’t have survived a double-lung transplant as well. Looking back, I’m grateful to have gotten the second opinion that’s turned into a second chance at life for me,” says Sarah of Laingsburg, Michigan.
It was 2011 when stomach pain and jaundice prompted her to go to the doctor. Twenty-nine years old at the time, doctors diagnosed Sarah with polycythemia vera, a rare blood disorder that causes the body to produce too many red blood cells, as well as Budd-Chiari syndrome, another rare condition where the veins that carry blood away from the liver develop blockages or become too narrow. Since blood clotting is a risk of polycythemia vera, it can cause Budd-Chiari syndrome, leading to jaundice and liver failure.
“When I was first diagnosed with my blood and liver conditions, my doctors told me the diseases would eventually lead to me needing a liver transplant,” says Sarah.
For nearly a decade, she was able to work with doctors closer to home to maintain her health and live a relatively good quality of life. That’s until they discovered Sarah had liver cancer in 2020.
“They caught the cancer very early, and I underwent radiation treatments. But with my liver function getting worse, I found out I needed that transplant earlier than I expected,” says Sarah.
Her care team in Michigan also made the discovery she has pulmonary hypertension – meaning she has high blood pressure in her pulmonary arteries, which carry oxygen-poor blood from the heart to the lungs. In Sarah’s case, she says they didn’t think medication could manage it, and she would ultimately need new lungs on top of the liver transplant.
“That’s when I decided to go to Cleveland for a second opinion. I didn’t want to also have a lung transplant and needed to know if there were other treatment options available for me,” says Sarah.
Once Sarah came to Cleveland Clinic, in Cleveland, Ohio, she first worked with pulmonologists Gustavo Heresi, MD, and Adriano Tonelli, MD, to try lowering her pulmonary pressures through medications. One of those medicines needed to be delivered through an IV and required her to be connected to a portable infusion pump 24/7. “I slept with it, showered with it – the pump couldn’t come out for any reason,” stresses Sarah.

Sarah had to carry around her portable infusion pump in a bag no matter where she went. It was needed to deliver medication for her pulmonary hypertension. (Courtesy: Sarah Minton)
On top of having to travel everywhere with an infusion pump, Sarah had fluid building up in her abdomen because of her liver disease. She was also experiencing a severe drop in her platelets, which are tiny cell fragments in the blood that help stop the bleeding if you’re injured. Her underlying conditions caused her to have an enlarged spleen as well. It took a multidisciplinary team of doctors to manage Sarah’s condition, and after two years, her lung function had improved. She could start being considered for a liver transplant and was eventually referred to critical care specialist Matt Siuba, DO, who had recently started a consultation service to evaluate patients with pulmonary hypertension to ensure it would be safe for them to undergo a transplant procedure.
“Patients with pulmonary hypertension have a higher risk when they go into the operating room, so we offer a more involved testing protocol than what's typically done prior to transplantation to see if the heart can handle the stresses of surgery,” says Dr. Siuba.
In Sarah’s case, Dr. Siuba performed a right heart catheterization and echocardiogram (heart ultrasound) to measure the pressures of the blood vessels inside her lungs as well as her heart function. He says they then simulated some of the stresses of the operating room to see how her heart would withstand the surgery.
“Fortunately, Sarah responded well to all the tests. She didn't have any deterioration. In fact, she had what we call cardiac function reserve in case she got into trouble. The combination of all these factors made us feel she could safely undergo a liver transplant,” says Dr. Siuba.
While waiting on the transplant list, Sarah had frequent doctor visits to manage the fluid building up in her abdomen and her declining platelet counts. Having no energy or appetite, these months were the hardest for Sarah, and she was preparing for the worst-case scenario.

Sarah experienced ascites because of her liver’s condition, which is a buildup of fluid in the abdomen.(left) Due to complications along the way, Sarah had frequent stays in the hospital.(right) (Courtesy: Sarah Minton)
“My parents sat me down one day and said, ‘If you don’t get this call for a liver transplant, we need to know what you want for your funeral arrangements.’ And they were right. It felt like the end was near, and I wasn’t sure if I was even going to make it to see my youngest daughter graduate high school,” says Sarah.
At first, Sarah’s doctors thought she could potentially receive a partial liver from a living donor. And after testing showed some close family members weren’t a match, they started spreading the word she needed a donor. When it comes to living donor liver transplants, up to two-thirds of the liver can be safely removed as long as the tissue is healthy and able to regenerate.
Sarah says more than 170 people applied to be living donors. However, her care team pivoted based on her condition and decided she would need a whole liver – which could no longer come from a living donor. But with the word Sarah needed a liver already out, the call that changed her life came.
“My dad got a call one day from someone whose family member had just passed away. They happened to be an organ donor, and the family wanted to donate their loved one’s liver to me,” says Sarah.
At the end of the day, Sarah knew the chances of this donor’s liver being compatible for her were slim. Thankfully, the odds were in her favor – the deceased donor was a match.
“I couldn’t believe it. We all cried happy tears. But it also comes with great sadness because I know this family just lost someone they loved,” says Sarah.
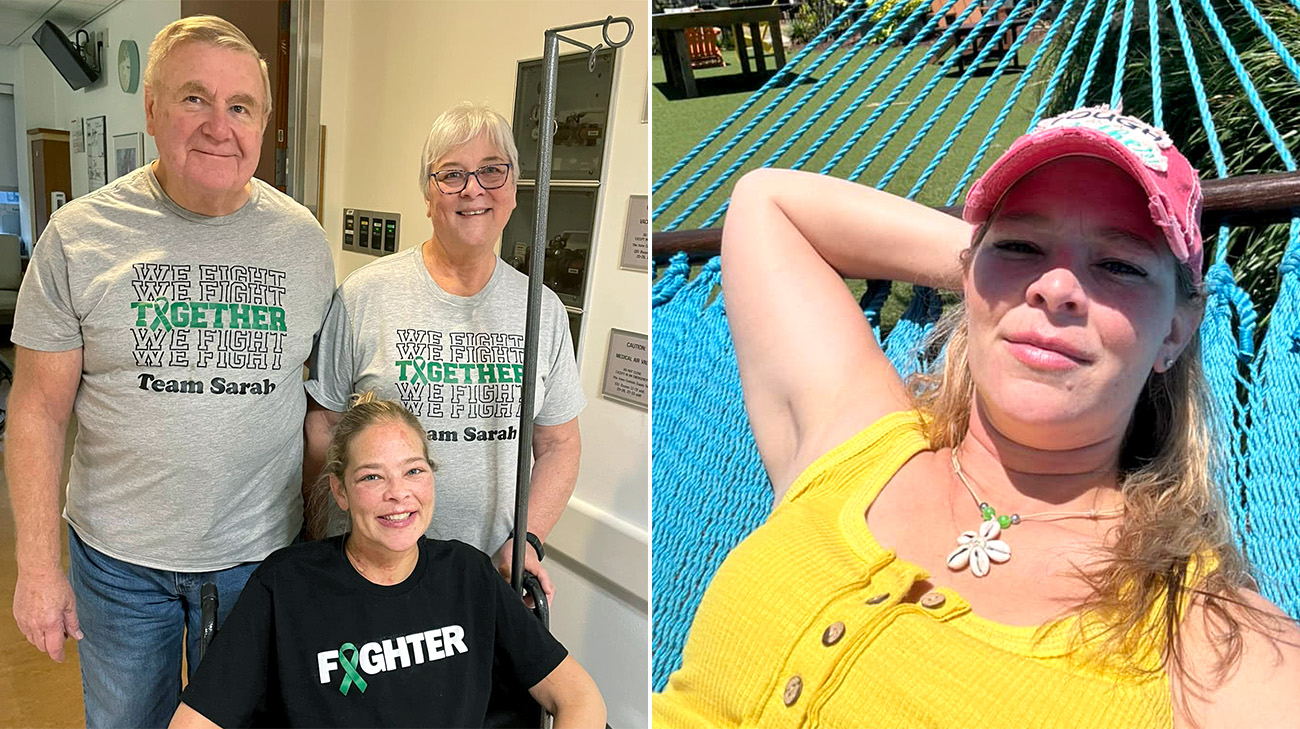
After over a month in the hospital following her transplant, Sarah was able to start her recovery at home and begin doing the things she loves again. (Courtesy: Sarah Minton)
In 2023, Sarah underwent the liver transplant performed by Koji Hashimoto, MD, PhD, the Director of Liver Transplantation at Cleveland Clinic. The surgery went well, but Sarah did experience some bleeding complications due to her low platelet count. She remained in the hospital for a month and a half.
“Once I came home, my recovery was really fast. I started walking further and further distances, my energy improved. Within five months, I was able to do even more than I could before the transplant because I felt that much better,” says Sarah, who adds finding ways to stay positive throughout this entire process also helped with her recovery.
Around six months, Sarah reached another milestone. Her lungs were healthy enough she didn’t need her portable infusion pump anymore. No longer having to carry the medical equipment around with her, she was able to start independently enjoying life again.
“I wasn’t able to swim with the pump because I couldn’t get it wet. As soon as I no longer needed it, I jumped in the pool. I was so excited I could finally swim again,” says Sarah.
Sarah continues following up with her care team to manage her blood condition and pulmonary hypertension. She’s thankful her doctors were willing to work with her, and she was able to avoid a double-lung transplant.
“If I didn’t have this team, I don’t know if I would have made it. They saved my life, and I can’t thank them enough,” says Sarah.
Dr. Siuba adds, “To put her through two operations would have been even more difficult for her, especially when you take into account she has pulmonary hypertension and a low platelet count. We’re happy to see Sarah thriving.”

Sarah is now looking forward to creating new memories with her loved ones, including her fiancé. (Courtesy: Sarah Minton)
Since her liver transplant, Sarah celebrated her daughters’ 20th and 18th birthdays, purchased a house and got engaged – all things she says wouldn’t have been possible without her care team or donor.
“I can't say thank you enough to my donor and their family. I think of them and pray for them every day. I want them to know I'm doing everything I possibly can to live my life to the fullest for them. I'm just so grateful to have this second chance at life. Becoming an organ donor saves lives,” says Sarah.
Related Institutes: Digestive Disease & Surgery Institute , Respiratory Institute

