
Julianne Smith says she’s grateful to be alive after surviving a severe type of ruptured brain aneurysm with only about a 10% survival rate. “I was 38 years old when it happened, and it was very eye opening to me that no one is guaranteed tomorrow,” says Julianne.
The young mother of three was going about her daily routine when she passed out in the kitchen. Her 10-year-old daughter was home at the time and quickly dialed her father.
“When my youngest daughter called, I could hear Julianne coming to, and she was slurring her speech. I immediately thought she was having a stroke and called 911,” says Mike, Julianne’s husband.
Mike recalls Julianne complaining of head pain before passing out again and paramedics rushing her to a nearby hospital. After discovering the ruptured brain aneurysm, she was flown by helicopter to Cleveland Clinic main campus in Cleveland, Ohio, for treatment.
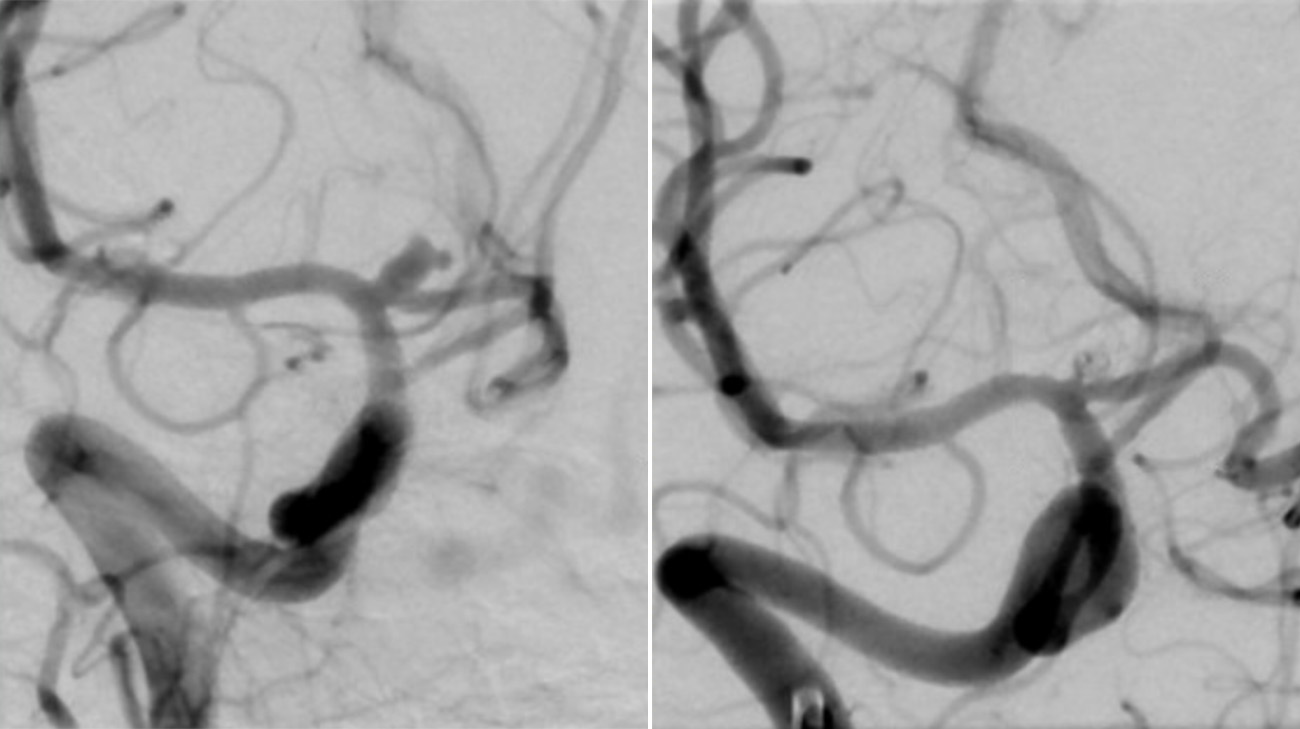
Imaging shows Julianne’s ruptured brain aneurysm before and after an endovascular coiling procedure to block blood flow into the aneurysm to prevent it from re-rupturing. (Courtesy: Cleveland Clinic)
“Julianne presented with the worst grade possible for a subarachnoid hemorrhage, which is when someone has a ruptured aneurysm or has some other reason for an artery bleeding in the head,” says Nina Zobenica Moore, MD, Julianne’s neurosurgeon.
Due to the subarachnoid hemorrhage, Dr. Moore says Julianne had increased intracranial pressure, which is a life-threatening condition that happens when there’s an imbalance between your brain tissue, cerebrospinal fluid and brain blood volume. Dr. Moore and the neurosurgery team quickly addressed this by draining excess fluid from the brain. Interventional neurologist Shazam Hussain, MD, then performed an endovascular coiling procedure to block blood flow into the aneurysm to prevent it from re-rupturing. Dr. Moore and team also worked closely with neurocritical care specialist Adam Barron, MD, and caregivers on the neuro intensive care unit to manage Julianne’s overall condition as she suffered from severe brain swelling, or cerebral edema.
“The first 24 to 48 hours when someone this sick comes into the hospital is really complicated. We had a number of different teams who were involved in her care, and Dr. Moore and I were in constant communication,” says Dr. Barron. “When the brain is under such pressure, physiology can change minute to minute. That means we had to quickly adjust to what we saw was happening in her body and brain to deliver the right medications and come up with a safe, effective plan.”
Because of how severe the brain swelling was, the neurosurgery team ultimately had to perform a right hemicraniectomy, where a large piece of Julianne’s skull was removed on the right side of her head to relieve pressure and allow the brain to swell out. But Julianne wasn’t out of the woods yet as she developed severe vasospasm.

A large portion of Julianne’s skull was removed after the brain aneurysm ruptured to relieve pressure. Her care team restored the skull following her recovery. (Courtesy: Mike Smith)
As many as 50% to 90% of people with an aneurysm rupture in the brain get vasospasm, which is when the blood that leaked out from the aneurysm irritates the blood vessels, causing them to constrict and narrow. Since this can potentially lead to a stroke, interventional neurologist Gabor Toth, MD, performed an angioplasty to open up Julianne’s vessels. This allowed blood to flow through more easily.
“Thirty percent of people don’t survive a ruptured aneurysm – many don’t even make it to the hospital. It took the fast action of a multidisciplinary team to successfully care for Julianne. It’s not just one person that got her through this, it was a whole group effort,” says Dr. Moore.
All in all, Julianne was in a coma for more than one week during her hospitalization. Throughout this difficult time, Mike says their family was comforted by the constant updates from her care team as well as other subtle signs from Julianne herself. “Even when she was out, she could still squeeze my hand like she knew I was there,” says Mike.
Once Julianne woke up, Mike remembers her personality immediately shining through, as Julianne made funny faces and did a peace sign in photos like her one daughter used to do. Julianne doesn’t remember much from her hospital stay but does recall the shock of learning about the events that took place.

Julianne makes a peace sign with her daughter while recovering in the hospital. (Courtesy: Mike Smith)
“I’m looking at the neurosurgeon, and I’m like, ‘How did this happen to me?’ I take pretty good care of myself, and I didn’t personally know anybody who had an aneurysm,” says Julianne.
Following the ruptured aneurysm, Julianne had trouble speaking and couldn’t move the left side of her body – preventing her from walking on her own. Since patients like Julianne are at a high risk for neurological issues, she underwent a rigorous rehabilitation process at Cleveland Clinic Rehabilitation Hospital in Beachwood, Ohio, as well as Cleveland Clinic Euclid Hospital’s Neuro Day program.
“Knowing what I know now about the severity of my rupture, I’m so grateful to even be here. I remember telling one of the therapists I have a lot to live for. I was so determined to get better,” says Julianne.

Julianne underwent months of rehab to relearn how to walk and regain her strength following the ruptured aneurysm. (Courtesy: Mike Smith)
Mike adds, “Once Julianne puts her mind toward something, she’s going to do it. When they’d tell her to do five steps at rehab, she’d do seven. That's just how she is, and I think that really helped.”
With hours of therapy, Julianne went from essentially being bedridden to walking freely again over the course of about six months. She also regained her ability to drive after temporarily losing it because of her mobility issues. Her speaking voice continues to get stronger as well.
“I’m back to doing the things I love, like volunteering and traveling. I’m able to drive my kids where they need to go again. I can go to our oldest daughter’s volleyball games. She just started high school, and it's all the firsts for our firstborn. I'm so grateful I'm still here to witness it,” says Julianne.
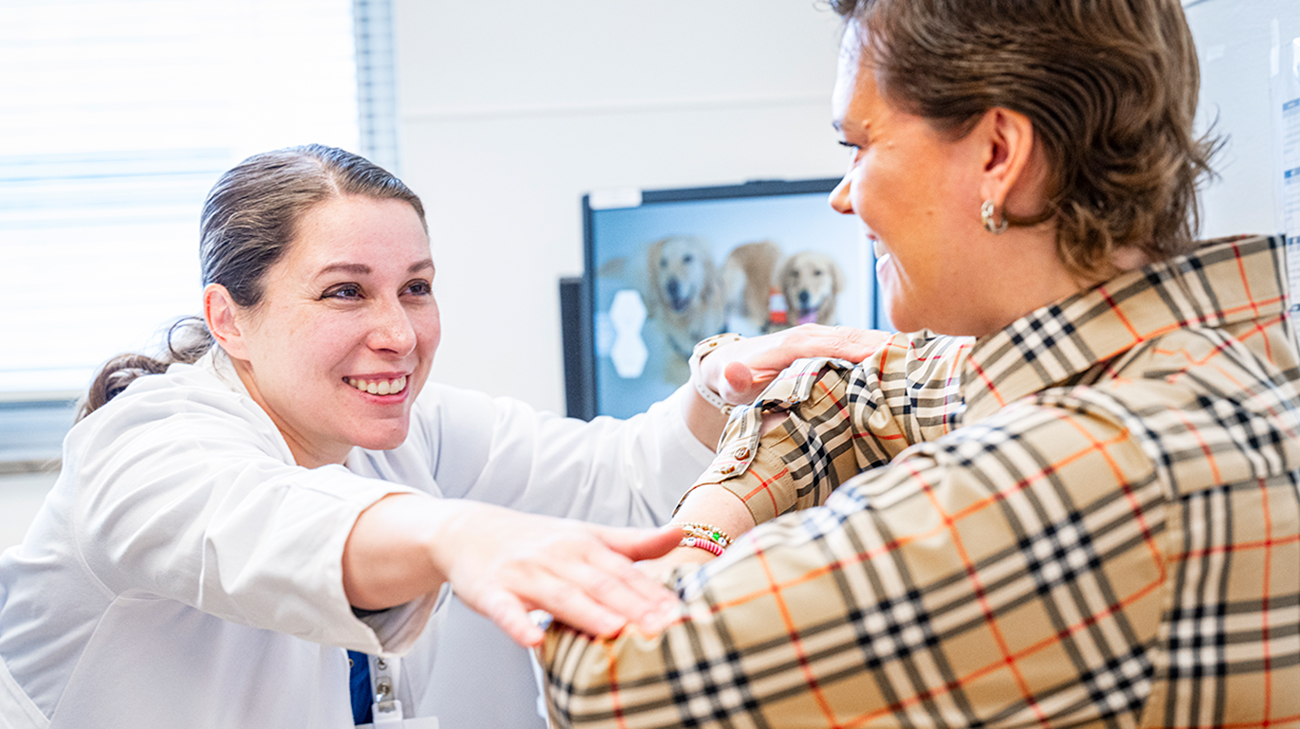
Julianne at a follow-up appointment with Dr. Nina Zobenica Moore. Julianne’s care team will continue to closely monitor her. (Courtesy: Cleveland Clinic)
Mike adds, “The physical therapists were phenomenal. They worked with Julianne and pushed her to get to where she is now. If you saw her walk into a room, you wouldn’t know she went through what she did.”
As Julianne reached new milestones, Dr. Moore was also able to restore the portion of Julianne’s skull she had to remove to alleviate her brain swelling. She’ll continue to closely monitor her moving forward. While Julianne wasn’t aware of any family history of aneurysms, Dr. Moore encourages others to touch base with their loved ones and keep tabs on any risk factors.
“It's easier to treat an aneurysm before it's ruptured, so tell your doctor if any of your family members have had an aneurysm. Not smoking and making sure your blood pressure is well managed can also help decrease the risk of a ruptured aneurysm,” says Dr. Moore.

Julianne with her family after months of recovery following the ruptured aneurysm. (Courtesy: Cleveland Clinic)
With a new outlook on life, Julianne isn’t taking one moment for granted. She’s looking forward to creating new memories with her family and more trips to Nantucket, Massachusetts – one of their favorite destinations. She’s thankful to her tight-knit church community for their prayers as well as others she didn’t even know who stepped up to support and pray for her. She’s also grateful to her care team who she credits for saving her life.
“From the first responders and flight medics to the doctors, nurses and physical therapists – everyone who took care of me was wonderful throughout this whole process. I'm so grateful to God everything lined up the way it did,” says Julianne.
Related Institutes: Neurological Institute

