
After spending nearly the entire first year of her life in the hospital, Adaya Robinson’s family is enjoying each moment with her at home. Despite everything she’s been through, Adaya’s mom says the 14 month old always has a smile on her face and is making progress that didn’t seem possible when she first found out her daughter had a rare congenital heart disease. Adaya was able to come home after undergoing a novel approach to treat her heart condition, allowing her to sidestep the need for a heart transplant.
“Adaya has defied the odds. She’s hit all of her milestones so far. She’s crawling and getting around wherever she wants to go,” says Christen Rachel, Adaya’s mom.
At around 20 weeks gestation, Christen learned Adaya had hypoplastic right heart syndrome, more specifically, pulmonary atresia with intact ventricular septum (PA-IVS) and right ventricle-dependent coronary circulation (RVDCC). PA-IVS accounts for less than 1% of congenital heart disease diagnoses, while RVDCC is exceedingly rare. With these conditions, the right side of Adaya’s heart was underdeveloped, and the heart was not getting oxygenated blood because of its structure.

Adaya spent nine months in the hospital because of her rare congenital heart disease. (Courtesy: Christen Rachel)
“I was scared. I had never heard of this condition before. I just started to prepare myself because I knew my life was going to change drastically,” says Christen.
After Adaya was born, she was taken to Akron Children's Hospital where she was initially seen by Robert Stewart, MD, cardiothoracic surgeon. It was determined she needed a heart transplant, and her care was transitioned from Akron Children’s Hospital (an affiliated program with Cleveland Clinic) to the Pediatric and Adult Congenital Heart Center at Cleveland Clinic. Adaya’s care team discovered she developed significant myocardial ischemia. The heart muscle was not getting enough blood to work as it should.
“Changes were showing up on the electrocardiogram when Adaya started crying. We had to act fast because even crying was putting stress on her heart, which could lead to cardiac arrest,” says Hani Najm, MD, a pediatric and congenital heart surgeon at Cleveland Clinic Children’s.
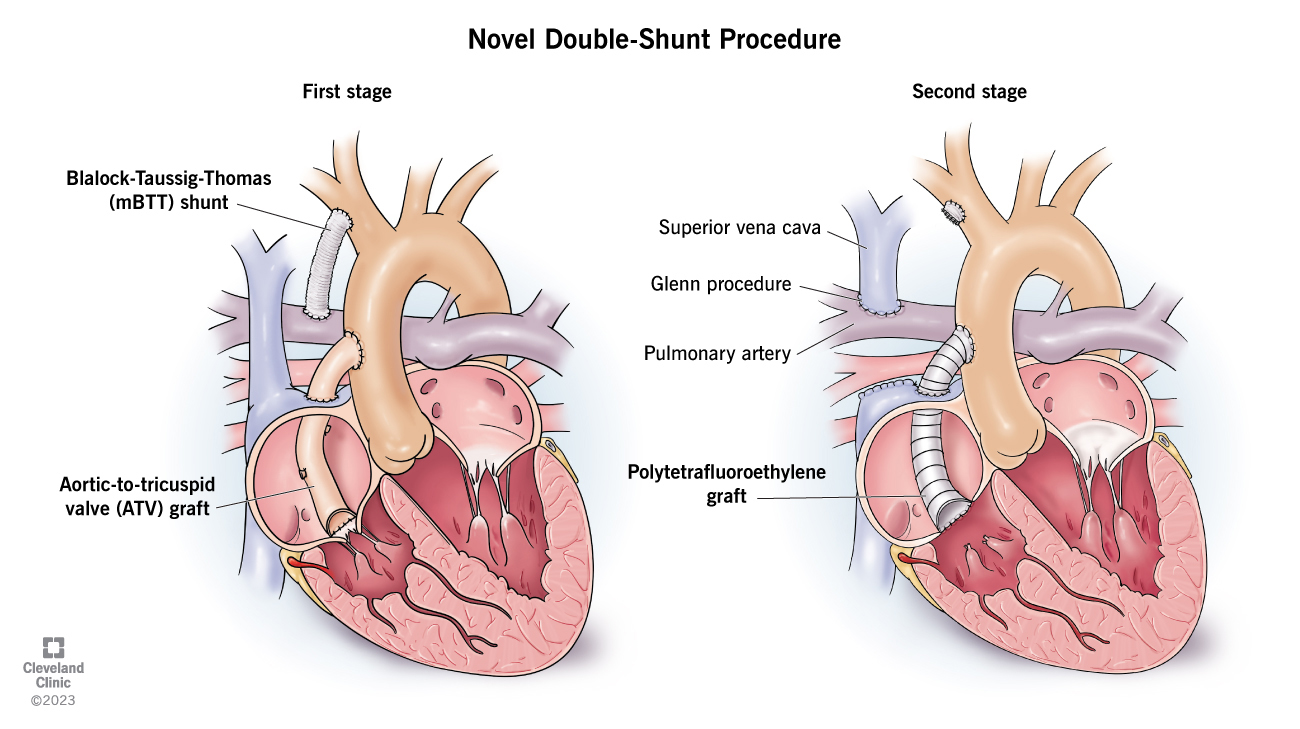
The first phase of Adaya’s treatment strategy involved installing a shunt as well as an aortic-to-tricuspid valve graft. During the second phase, the original shunt was replaced, and the aortic-to-tricuspid valve graft was upgraded. (Courtesy: Cleveland Clinic)
Quick thinking led Dr. Najm to create a three-phase novel strategy to correct Adaya’s blood flow. The first phase involved installing a shunt as well as an aortic-to-tricuspid valve graft. The shunt, or small tube, would increase blood flow to the lungs, while the aortic-to-tricuspid valve graft would help deliver oxygenated blood to the heart. After the procedure, Adaya was placed on a left ventricular assist device to help her heart pump blood.
“Three days later, it was clear her heart was working very well, and she no longer needed the ventricular assist device. She was stable in the pediatric intensive care unit,” says Dr. Najm.

Adaya’s care team included Dr. Hani Najm, who came up with the novel strategy to address her heart condition. (Courtesy: Cleveland Clinic)
Adaya remained on the heart transplant waiting list as her care team continued to monitor her condition. After six months of waiting, Dr. Najm says Adaya was at the age they would implement the second phase of the strategy and change the shunt they originally put in place. During Adaya’s second procedure, Dr. Najm also upgraded the initial aortic-to-tricuspid valve graft, which will likely remain intact until she becomes an adult.
“She was doing so well after this procedure. My team and I were confident keeping her own heart was the best treatment option. She was able to be taken off the transplant waiting list shortly after the procedure. This is the only case that has proven the aortic-to-tricuspid valve graft is sufficient enough, and a heart transplant would no longer be needed,” says Dr. Najm.

Now at home, Adaya is reaching all her developmental milestones and continues making progress. (Courtesy: Cleveland Clinic)
Christen had been driving more than an hour from her home in Mansfield, Ohio, to see her daughter in the hospital multiple times a week. She did this all while working and taking care of her two other daughters. After spending nine months in the hospital, it was a huge relief the day Christen learned Adaya would finally be able to come home.
“I found out around my birthday. The doctors told me Adaya had shown them how strong she was, and she would be able to come home. It seemed like I would never hear those words. It was one of the best moments of my life honestly,” says Christen.

Adaya’s care team will continue to monitor her condition until she grows enough to undergo a final operation called the Fontan procedure. (Courtesy: Cleveland Clinic)
Adaya came home for the first time in April 2023. She now enjoys playing with her older sisters and is slowly learning how to walk. Adaya’s care team will continue to follow up with her, and once she grows enough, she’ll undergo a final operation called the Fontan procedure. Her 15-year life expectancy after this procedure is expected to be better than if she had received a heart transplant.
“If I could thank Dr. Najm a million times over, I would. Dr. Najm and his team made getting through the hardest part of my life a little bit easier,” says Christen.
Dr. Najm is also thankful to Christen for putting her trust in him to try a new treatment approach that now has the potential to help many other patients in similar situations around the world.

Adaya’s mom, Christen, says she’s enjoying every moment with her daughter at home and making up for the months she was in the hospital. (Courtesy: Cleveland Clinic)
“The road to transplant can be difficult, and the risk of coronary compromise is high while patients await the procedure. Moreover, heart transplantation doesn’t come without a cost, and timely access to transplant organs – particularly for infants – remains an issue,” says Dr. Najm. “In some parts of the world, a heart transplant is not even a viable option for care. We hope this novel approach will not only prevent the need for transplant but may also improve longer-term outcomes in patients with right ventricle-dependent coronary circulation.”
Related Institutes: Heart, Vascular & Thoracic Institute (Miller Family), Cleveland Clinic Children's

