A sacrocolpopexy is a surgical procedure that treats pelvic organ prolapse. Pelvic organ prolapse occurs when the muscles and tissue that support your pelvic organs become weak or damaged and slip out of position. During sacrocolpopexy, your surgeon uses surgical mesh to lift your organs back into place.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Video playlist content: This video playlist is available to watch online.
View video playlist online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_yq8vebvx/flavorId/1_5f3sgelj/format/applehttp/protocol/https/a.mp4)
Sacrocolpopexy
A sacrocolpopexy is a surgical procedure to treat pelvic organ prolapse. Pelvic organ prolapse is when one or more of your pelvic organs slips down into your vagina. It happens when the muscles and tissues that normally support your pelvic organs become weak or damaged. During a sacrocolpopexy, your surgeon lifts the affected organs back into place and secures them with surgical mesh. Restoring your pelvic organs to their normal position helps relieve side effects of prolapse like bulging, pelvic pressure or urinary incontinence (leaking pee).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Most surgeons perform sacrocolpopexy laparoscopically using small incisions and a camera. Some surgeons perform laparoscopic sacrocolpopexy with the help of a robot.
Sacrocolpopexy treats the organs in your pelvis: specifically, the area between your left and right hip bones and your pubic bone and tailbone. Examples of pelvic organs include your vagina, uterus, cervix, bladder, urethra (the tube that you pee out of), intestines and rectum.
These organs are held in place by a group of muscles called your pelvic floor as well as ligaments from your vagina to your backbone. Your pelvic floor acts like a hammock for your pelvic organs. When this support system becomes stretched, weakened or torn, it allows pelvic organs to slip out of their normal places or sag down as the ligaments usually will stretch over time. This is pelvic organ prolapse. Sacrocolpopexy addresses organs slipping into your vagina.
There are different types of prolapse, depending on the organ or organs involved. These include:
Advertisement
Some of the most common symptoms of pelvic organ prolapse are:
The most common causes of pelvic organ prolapse are the following:
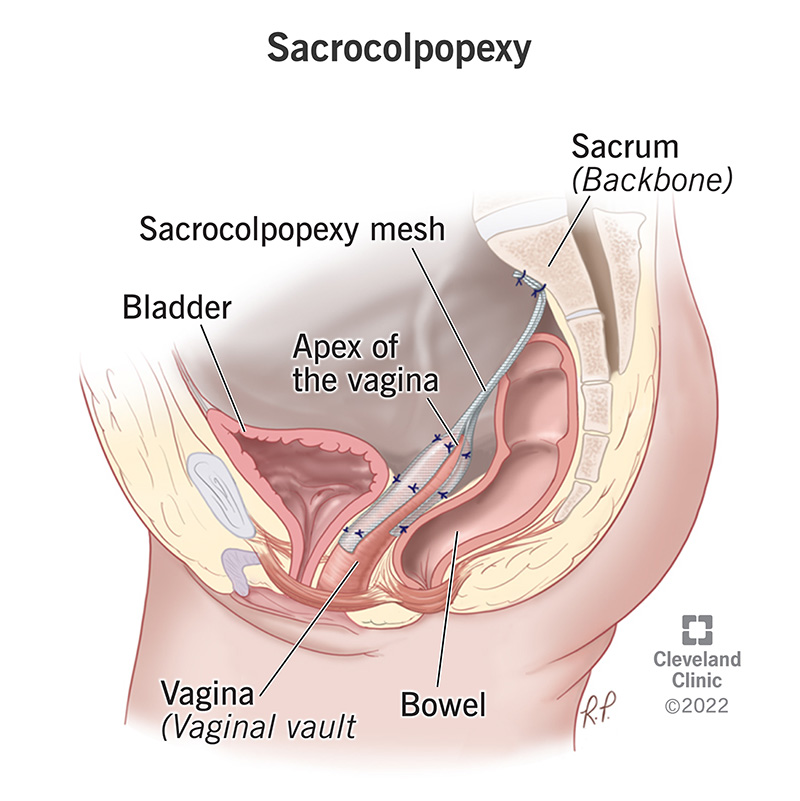
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17939-sacrocolpopexy)
In a sacrocolpopexy procedure, a surgeon attaches a special type of surgical mesh from your upper vagina to your sacrum (tailbone), creating a bridge or synthetic ligament. First, the bladder and rectum must be separated from the vagina to create a space to place the mesh. Next, the surgeon places surgical mesh at the top and bottom walls of your vagina. Finally, they attach it to a ligament covering your sacrum. Because your sacrum is higher than your vagina, the mesh acts as a lift.
Your surgeon may remove your uterus (hysterectomy) and/or your fallopian tubes and ovaries during sacrocolpopexy. Removing these organs eliminates your risk for uterine cancer and reduces your risk of developing ovarian or fallopian tube cancer. Your surgeon determines if removing your uterus is appropriate based on your health history, cancer risk and preference.
Most healthcare providers ask you to arrive several hours before your scheduled surgery time. Be sure to call your provider if you haven’t received pre-operative instructions. These instructions usually contain specifics about when to stop eating and drinking the night before surgery, stopping certain medications and more.
Some examples of pre-op instructions include:
Most surgeons perform a sacrocolpopexy laparoscopically (through small incisions, or cuts) in the following way:
Advertisement
For robotic-assisted sacrocolpopexy, your surgeon follows similar steps, but they pass robotic controllers through small incisions. Your surgeon guides these small instruments during the procedure.
The surgery takes two to four hours to complete. When it’s over, you’re taken to a recovery area to wake up from the anesthesia. You'll stay in the recovery room until the anesthesia wears off. If your surgeon has any concerns about the surgery, you may need to stay overnight for observation.
Next, your healthcare team performs a voiding trial. Before surgery, your healthcare provider placed a catheter into your bladder. A catheter is thin tube that removes pee from your bladder. A voiding trial checks to see if you can empty your bladder without a catheter. During a voiding trial, your provider fills your bladder with saline and removes your catheter. If you can pass (or void) two-thirds of the saline, you’ll be sent home without a catheter and can pee normally.
If you’re unable to empty your bladder (pee on your own), you may need to use a catheter at home for a few days. Your provider will give you instructions on how to replace and care for your catheter at home. Your provider will schedule an appointment for you to complete another voiding trial in a few days.
Advertisement
Your surgeon will close your incisions with either glue or tape. You should keep the incisions clean and dry. Any stitches underneath your skin will dissolve on their own. Be sure to wash your hands often, especially before touching your incisions or changing out bandages on your incisions. Your healthcare provider will advise you on how to care for your incisions.
Recovery from surgery usually takes about six to eight weeks for most people. Your provider should give you post-operative instructions that detail things like modifying your activities, taking care of yourself or taking medications.
Your healthcare provider will schedule a follow-up appointment within two weeks of surgery to make sure the procedure was successful and that you’re healing well.
Advertisement
Sacrocolpopexy is safe, but all surgeries have risks. There have been complications with using mesh to repair pelvic organ prolapse when surgeons perform the repair vaginally. For this reason, surgeons now only use mesh for pelvic organ prolapse through a person’s abdomen. If you’ve had surgery to repair prolapse using mesh through your vagina, contact your provider if you notice any unusual symptoms or problems.
As with all surgical procedures, there are risks to sacrocolpopexy. Discuss the procedure with your provider so you understand the risks. Some of the risks include:
You may also experience side effects from anesthesia after the procedure. Things like nausea or vomiting, tiredness and confusion are all normal side effects for the first 24 hours after surgery.
Gas pain and abdominal swelling are also common side effects from the gas that inflates your abdomen during the procedure.
Recovery from sacrocolpopexy takes about six to eight weeks. Your provider will ask you to refrain from certain activities like heavy lifting or sexual intercourse for a specific amount of time. Be sure to check with your provider about any lifestyle changes you should make while you recover.
Sacrocolpopexy is often an outpatient procedure, which means you can go home the same day. In some cases, your healthcare provider may ask you to stay overnight. Several factors go into this decision, such as the severity of your prolapse, if there were complications during surgery or if you have other medical conditions.
The success rate for this procedure is high — around 90%. Factors like the extent of your prolapse, which organs were affected and the surgical method could impact the success of sacrocolpopexy.
It’s important to understand that prolapses can come back. Taking steps like maintaining a weight that's healthy for you, avoiding straining to poop and not lifting heavy objects can all help avoid another prolapse.
Call your provider if you begin to feel symptoms of pelvic organ prolapse after surgery. In some cases, surgery isn’t successful and your provider may need to treat your condition in another way.
You should contact your provider if any of the following happen:
Sacrocolpopexy is a common procedure to treat pelvic organ prolapse. There are several different treatments for pelvic organ prolapse that your healthcare provider may suggest. Take time to understand your options and the risks and benefits of each. Sacrocolpopexy is a highly successful procedure that lifts your pelvic organs back to their usual position within your pelvis. This relieves pelvic organ prolapse symptoms. Discuss this procedure with your provider to make sure it’s right for you.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
From routine pelvic exams to high-risk pregnancies, Cleveland Clinic’s Ob/Gyns are here for you at any point in life.
