Polyarteritis nodosa or PAN is a rare condition of inflamed blood vessels that hurt your organs. You can have symptoms in many parts of your body at one time. Prompt treatment with medicine gives you the best chance at remission, but relapses can happen. Affected sites and the severity of your condition play a role in your outlook.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
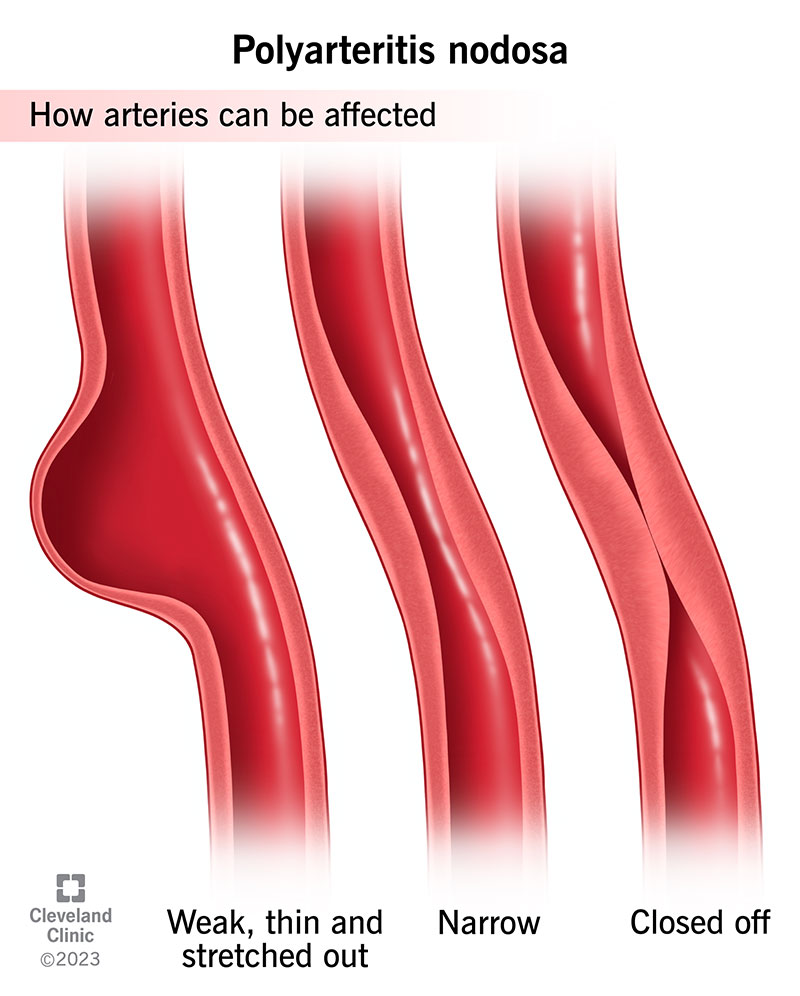
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/polyarteritis-nodosa)
Polyarteritis nodosa (PAN) is a rare condition in which blood vessel inflammation (vasculitis) injures your organs. Inflammation can make a blood vessel:
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Although PAN mainly affects medium-sized blood vessels, affected organs may lose some or all of their ability to function.
Polyarteritis nodosa most commonly affects your:
Most people have issues with more than one area of their body with PAN. Rarely, you may only have symptoms in your skin (cutaneous PAN). Your provider will need to keep checking on you to make sure you don’t develop symptoms in other parts of your body.
Polyarteritis nodosa usually doesn’t cause symptoms in your lungs.
Polyarteritis nodosa is very rare. Out of a million people in the United States, fewer than 10 people per year get a polyarteritis nodosa diagnosis. The same is true in England.
PAN can affect many different parts of your body with a wide range of symptoms. Polyarteritis nodosa symptoms may include:
Advertisement
Healthcare experts don’t know the cause of polyarteritis nodosa. It may have a genetic (inherited) cause or a connection to various blood disorders in some people.
Research strongly supports that your immune system plays a critical role in PAN. It does this by causing blood vessel and tissue inflammation and damage.
A hepatitis B (and sometimes hepatitis C) infection may set off polyarteritis nodosa. Rates of polyarteritis nodosa have decreased significantly since the creation of the hepatitis B vaccine.
Polyarteritis nodosa risk factors include:
Complications may include:
To make a polyarteritis nodosa diagnosis, a provider will use information from:
A provider may order these tests:
Polyarteritis nodosa treatment uses medications that suppress your immune system.
The goal of treatment is to get rid of inflammation. When you do this, providers say you’re in remission. Once your condition improves, you’ll slowly reduce your medication dose and eventually stop taking it.
If PAN affects your critical organ systems, you’ll take more than one medicine. Polyarteritis nodosa treatment will include:
People with certain types of cancer may receive high doses of cyclophosphamide. But people with vasculitis get cyclophosphamide doses that are 10 to 100 times lower than the amount that treats cancer. In people with polyarteritis nodosa, the drug slows down their immune systems so they don’t cause inflammation.
Usually, you only take cyclophosphamide until remission (around three to six months). Then, you may switch to another immunosuppressive agent like methotrexate or azathioprine to maintain remission.
Different people take a maintenance immunosuppressive medication for different lengths of time. Most people take it for at least one to two years before a provider will consider slowly reducing their dosage and stopping it.
Advertisement
In rare instances, people might do well with corticosteroid therapy alone if polyarteritis nodosa doesn’t affect their nervous system, heart, kidneys or intestinal tract.
People who have a PAN-like vasculitis associated with hepatitis B may also take antiviral medications to treat the hepatitis.
Immunosuppressive medications can have side effects like mood changes, infection or swelling. Watching for side effects helps prevent or minimize them. You may tolerate treatment at first, but then not do well over time. This makes it important to do ongoing monitoring. In some cases, you may need to watch for long-term effects even after stopping the medication.
It can be harder to fight an infection while taking immunosuppressants. Vaccines can help you lower your risk of getting an infection like the flu or pneumonia.
For some people, polyarteritis nodosa comes on little by little. For others, it can get worse quickly and be fatal in just a few months. People who have symptoms in their digestive systems, hearts, kidneys and/or central nervous systems have a worse prognosis than those who don’t.
Although polyarteritis nodosa can be a sudden and serious illness, many people with PAN do extremely well. The severity of your illness affects how well you do. But you can achieve remission even with the most severe polyarteritis nodosa if a provider treats you promptly and monitors you closely.
Advertisement
After achieving remission, polyarteritis nodosa can recur or relapse. Estimates of the rate of relapse for PAN vary widely but range from 10% to 40%. Symptoms during relapses may be similar to what you experienced at the time of your diagnosis or they may be different. The treatment for relapses is like that of a newly diagnosed disease. Most people with polyarteritis nodosa can achieve remission again.
If you get treatment for polyarteritis nodosa, you have at least an 80% chance of living another five years. If you don’t get treatment, your five-year survival odds drop to less than 15%.
You can’t change some of the things that put you at risk for polyarteritis nodosa, like age. But a vaccine can protect you from the hepatitis B infection that can set off PAN in some people.
You can lower your chances of having a severe relapse by:
Contact your provider if you have some of the symptoms of PAN. But if you have chest pain and shortness of breath, seek immediate care.
You may want to ask your healthcare provider:
Advertisement
It can be hard to manage the symptoms of polyarteritis nodosa and deal with side effects from medications. Seek out a counselor if you need to talk to someone who understands your situation. Don’t be afraid to ask your provider about anything that isn’t clear.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Vascular disease may affect your life in big and small ways. Cleveland Clinic’s specialists treat the many types of vascular disease so you can focus on living.
