Enthesopathy causes pain and other symptoms where your tendons and ligaments connect to your bones. Enthesitis (inflammation at one of these points) is the most common type. Lots of injuries and health conditions that cause inflammation in your connective tissue can cause enthesopathies. Treating or managing the cause will relieve your symptoms.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
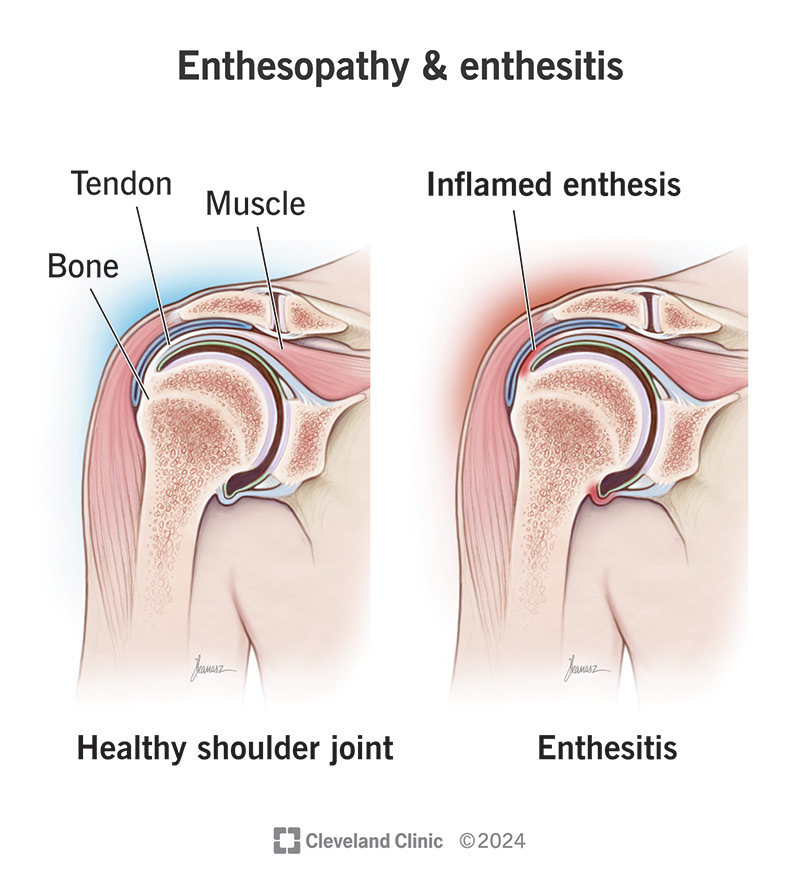
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/enthesopathy-enthesitis)
Enthesopathy is a broad term for any health condition or injury that affects the places tendons and ligaments connect to bones throughout your body.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Tendons and ligaments are both strong, flexible bands of tissue. Tendons connect muscles to bones. Ligaments connect bones to bones.
An enthesis is the medical name for the exact location on a bone where a tendon or ligament connects. The suffix “-pathy” at the end of a word means a disorder or issue that affects that body part. So, enthesopathy is something wrong with one or more of your entheses and that connective tissue.
Enthesopathy is any condition or disorder that affects an enthesis. Enthesitis means there’s inflammation in an enthesis. Enthesitis is a specific type of enthesopathy.
Healthcare providers sometimes use the terms as interchangeable names for the same issues. Your provider will suggest treatments to manage the symptoms you’re experiencing and will diagnose what’s causing them — no matter which word they use to describe it.
It’s hard for experts to estimate exactly how many people experience enthesitis each year. That’s because ligament and tendon pain and swelling are such common symptoms — especially after injuries. Also, many people with enthesopathies get better before they get an official diagnosis.
Experts know for sure that enthesitis is very common among people who have inflammatory arthritis like psoriatic arthritis and ankylosing spondylitis. In fact, someone having enthesitis more than once is one clue providers use to diagnose these conditions.
Advertisement
The most common enthesitis symptoms include:
Some people with enthesopathies also experience changes in their fingernails and toenails. You might notice pitting (little bumps or divots in your nails) or discoloration.
Enthesitis can affect any tendon or ligament connection in your body, but some common places include your:
Two issues cause all types enthesopathy (including enthesitis):
Some injuries that cause enthesopathies include:
Health conditions that create inflammation can trigger enthesitis. Your immune system responds to certain conditions by creating a special type of protein called cytokines. Cytokines help your body heal, but they also cause inflammation. Some conditions that trigger the inflammation that leads to enthesitis include:
People with chronic enthesopathy (repeated cases that come and go) have an increased risk of developing bone spurs. The cytokines that cause enthesitis inflammation can also trigger your bones to grow new tissue by mistake. Bone spurs can increase or cause more severe pain.
A healthcare provider will diagnose enthesopathy with a physical exam. They’ll examine the area where you’re experiencing symptoms and might lightly press on your skin (palpitation). Tell your provider when you first noticed pain, stiffness or other symptoms, and if any activities seem to make them worse (or better).
There’s no test that can diagnose enthesitis, but your provider might use an imaging test to take pictures of your body to look for injuries or inflammation, including:
You might need blood tests if your provider thinks you have certain inflammatory conditions.
Which treatments you’ll need will depend on what’s causing the enthesitis. You may only need at-home treatments to help your body heal after an injury, or you might need a long-term management plan for a chronic condition. The most common enthesopathy treatments include:
Advertisement
Treating enthesopathy is less about curing a disease than it is about managing it when it happens. It’s not like taking antibiotics to cure a bacterial infection. Treating enthesopathy and the injury or condition that caused it can make it go away completely.
You might have enthesitis that comes and goes in episodes of symptoms called flares or flare-ups — especially if you have an autoimmune disease that causes it. Your provider will help you manage the symptoms you experience and find ways to reduce how often they affect you.
Everyone’s outlook is different. It depends on which type of enthesopathy you have and what’s causing it.
If you have an injury, there’s a very good chance the enthesitis will go away once your body heals and you modify your activities. You should be able to resume all your usual activities with no long-term side effects. Don’t resume intense physical activities until your provider says it’s safe to, even if you start to feel better.
Some health conditions that can cause enthesopathy are chronic (long-lasting). You’ll have to manage these conditions for a long time, maybe even the rest of your life. Your provider will tell you what to expect and suggest ways to manage these conditions.
Advertisement
You usually can’t prevent enthesitis. Injuries that happen unexpectedly and health conditions you can’t avoid cause it. Talk to your healthcare provider about the best ways to manage any conditions you have. You might be able to reduce your risk of enthesitis flares, but not always prevent them.
Visit a healthcare provider if you experienced an injury or notice changing or worsening pain, swelling or can’t move a joint. Tell your provider if it seems like your enthesitis treatments aren’t working as well as they used to, of if you’re having flare-ups more often. They might be able to adjust or change your treatments.
Questions you may want to ask your provider include:
No, enthesopathy and arthritis are different issues. But they can be closely related. There are more than 100 types of arthritis, and most of them cause pain, stiffness and swelling that might feel like enthesopathy.
Also, many types of inflammatory arthritis can cause enthesitis, so having it can increase your enthesitis risk. Talk to your healthcare provider about which symptoms or changes to watch out for.
Advertisement
Enthesitis and enthesopathy affect specific parts of your tendons and ligaments. And you probably haven’t considered what or where an enthesis is in your body until one starts hurting. Whether or not you can point to any of your entheses on an anatomical diagram, the pain and stiffness from enthesitis can have a big impact on your daily routine.
Enthesitis can be a one-time issue after an injury, but a chronic condition you may have to manage for a long time can also cause it. Ask your provider any questions you have. They’ll help you help you understand what’s causing the symptoms you’re experiencing, how you can relieve them and what you’ll need to do to manage the cause.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.