Batten disease is a group of genetic conditions that cause cells to collect waste instead of getting rid of it. This leads to seizures, vision loss and problems with thinking and movement. Symptoms get worse over time. It leads to early death for children. There’s no cure for Batten disease but research is ongoing to learn more.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Batten disease is a group of genetic conditions that cause waste material to build up in your child’s brain cells. It affects the structure and function of cells (neurodegeneration) and ultimately causes their death. Batten disease is fatal.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
You may hear your child’s healthcare provider refer to Batten disease as neuronal ceroid lipofuscinosis (NCL).
All types of Batten disease cause many of the same symptoms like seizures, vision loss and cognitive (thinking and reasoning) problems. Symptoms can appear in babies, children and teenagers and get worse with age.
There’s no cure for Batten disease. Healthcare providers focus on treating symptoms and improving your child’s quality of life.
There are 14 known types of Batten disease grouped into categories based on the age when symptoms begin. Symptoms may start in infancy, late infancy, childhood or the early teenage years.
The name for each type of Batten disease starts with “CLN.” This stands for “ceroid lipofuscinosis, neuronal” — the name of the affected gene. The name ends with a number from 1 to 14.
The most common type of Batten disease is CLN3 (juvenile Batten disease). Symptoms of CLN3 usually begin between ages 5 to 15.
Healthcare providers estimate that Batten disease affects about 3 of every 100,000 babies born in the United States.
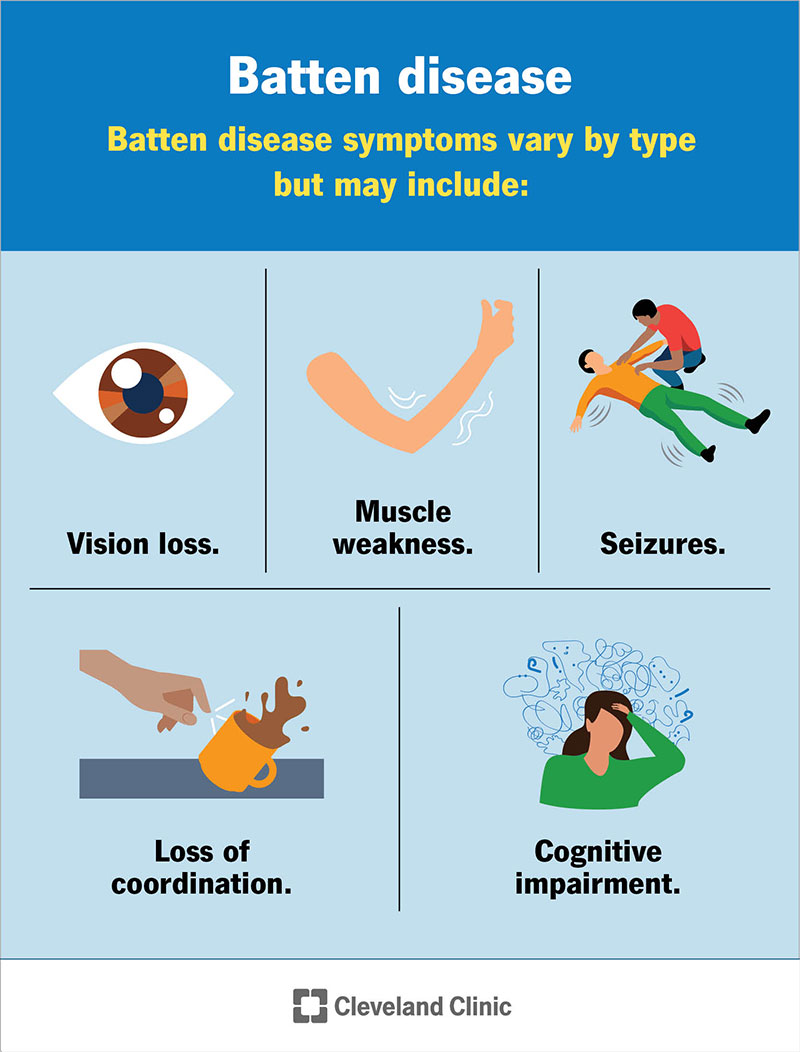
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/6018-batten-disease)
All types of Batten disease share many of the same symptoms, but they may begin at different ages. The first signs and symptoms of Batten disease include:
Advertisement
Other symptoms may include:
Babies and children with Batten disease grow and develop as expected for a period of time. They meet developmental milestones, such as crawling, walking, talking and feeding themselves. But then, they stop progressing and lose learned skills. Symptoms usually worsen quickly for young children.
A gene change (mutation) to a CLN gene causes Batten disease. This gene is responsible for breaking down and getting rid of cell waste. When a CLN gene variant happens, your child’s body isn’t able to clean up waste, so it collects in their cells. Lipids (fats), sugars and proteins build up in cells all over their body. The most affected cells are brain cells.
The buildup of waste within your child’s body causes it to stop working properly. Their nervous system isn’t able to do its job around the waste, which leads to life-threatening symptoms.
Yes, Batten disease is an inherited metabolic disorder. You’re more likely to develop Batten disease if your biological parents are carriers of the genetic variant that causes it. Your parents won’t have symptoms if they only carry one copy of the genetic variant.
It’s autosomal recessive. This means that both biological parents need to carry and pass the gene variant on to a child for the child to develop symptoms.
Batten disease leads to early death in infants, children and young adults. Symptoms will progressively get worse. For example, vision loss leads to blindness and muscle weakness leads to paralysis. Since cells die off due to a waste buildup, they aren’t able to function. This affects how your child’s organs perform. If their organs don’t have the support from their cells to do their jobs, organ failure is an expected outcome.
A healthcare provider will diagnose Batten disease after a physical exam and testing. They’ll learn more about your child’s symptoms and biological family medical history during the exam. Testing may include:
Advertisement
Other blood and imaging tests may be necessary to rule out conditions with similar symptoms.
There isn’t a cure for Batten disease. Treatment instead focuses on symptom management and support for you, your child and your family.
A team of healthcare providers will offer a variety of treatments for the many symptoms of Batten disease including:
Advertisement
For example, providers may prescribe medications to regulate seizures or to prevent hallucinations. Physical therapy can relieve muscle spasticity and help children retain mobility.
Mental health and family counseling are essential after receiving a Batten disease diagnosis. This condition leads to early death, and it can take a toll on you and your family. There are also support groups and bereavement support groups available to connect you and your family with others who share a similar experience and help you manage grief.
Researchers are studying many promising treatments for Batten disease. These include medications, stem cell transplants and gene therapy to replace the gene variant. Your child’s provider might recommend participating in clinical trials (tests on humans). Until other treatments for Batten disease are available, healthcare providers focus on treating the symptoms of the condition.
Currently, there’s one FDA-approved treatment for children with CLN2. Children receive infusions of a medicine called cerliponase alfa (Brineura®) every two weeks. Providers inject the medicine directly into the fluid surrounding your child’s brain. The medicine slows down the progression of mobility symptoms, like the loss of the ability to crawl or walk (ambulation). However, it doesn’t slow down other symptoms.
Advertisement
The prognosis (outlook) is poor for Batten disease. It’s fatal and leads to early death for children diagnosed with the condition. Symptoms progressively get worse within weeks to months to years. Eventually, your child will become blind and won’t be able to communicate, walk, sit independently and interact with others. The speed of symptom progression varies from one child to the next.
It’s devastating to receive this outlook, but your child can still participate in and enjoy childhood activities until their body tells them it’s time to slow down. Your child will need extra love and support throughout their life. You’ll get to know your child’s care team well since you can expect frequent office visits to manage your child’s symptoms as they progress. Their care team is available to answer any questions you might have along this journey.
In addition to supporting your child, you and your family will need support, as well. It isn’t easy to plan for a loss and then to experience one. No matter what you do to prepare, it feels like you’re losing a piece of yourself, and that’s not easy to deal with on your own. Reach out to a mental health professional or your primary care physician (PCP) if you need support through this difficult time. You may participate in therapy, family counseling or join a support group.
Most children diagnosed with Batten disease survive until early adulthood. Your child’s outlook varies based on the disease type and severity. For example, infants and young children usually have a five-to-six-year survival rate after symptoms begin. If your child develops symptoms around age 10, they may live into their early 20s. The earlier symptoms appear, the shorter the lifespan.
End-stage Batten disease is when your child needs around-the-clock care due to severe symptom progression. At this stage, your child may not be able to move or get out of bed. They may lose their sight completely and won’t be able to hold a conversation with you.
This is the most challenging stage of Batten disease. Healthcare providers will do everything they can to keep your child comfortable. Your child’s body is slowly shutting down during this final stage.
It isn’t possible to prevent Batten disease. If you have a family member or child with the condition, talk to your provider about genetic counseling. If you’re planning on becoming pregnant, you may choose to get a genetic test to see if you and your partner both have the gene that causes Batten disease. A healthcare provider can help you plan for a pregnancy.
If your child has signs of Batten disease, see their provider right away. An early diagnosis can greatly improve your child’s quality of life.
If you have a family member with Batten disease, talk to your provider about genetic counseling if you plan on expanding your family. A genetic test can tell if you and your partner both have the gene that causes the disorder.
Questions you may want to ask your provider include:
Yes. It’s very rare, but adults can develop symptoms of Batten disease. It usually happens around age 30. Adults who develop Batten disease usually have mild symptoms. Adult symptoms don’t shorten your life expectancy.
No one wants to hear that their child has a fatal condition that’ll prevent them from reaching adulthood. You might feel hopeless, depressed, unbearably sad or frustrated as you deal with this diagnosis. It’s normal to have these feelings. Your child’s care team may recommend visiting a genetic counselor to learn more about Batten disease, what you can expect and how you can help your child and your family through this process.
As you care for your child, it’s important to remember that you’re not alone. Although there’s no cure for Batten disease, researchers are continually working to develop treatments. Healthcare providers are studying multiple promising medications that can slow the progression of symptoms and improve your child’s quality of life.
Ask your provider about joining a support group or network of other parents who have children with the condition. Sharing your experiences and learning from others can be incredibly helpful and comforting.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
As your child grows, you need healthcare providers by your side to guide you through each step. Cleveland Clinic Children’s is there with care you can trust.
