Fragile X syndrome is the leading cause of inherited intellectual disabilities. There are behavioral, physical, intellectual and mental health symptoms. Although there isn’t a cure, medication and therapy can help manage symptoms.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Fragile X syndrome (FXS) is an inherited genetic disorder that causes physical abnormalities, behavioral issues and a wide range of other health problems, including:
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Fragile X syndrome is the most common form of inherited intellectual and developmental disability (IDD). It gets its name because when you look at the X chromosome through a microscope, part of it looks “broken” or “fragile.” Another name for the condition is Martin-Bell syndrome.
Researchers don’t know the exact number of people with fragile X syndrome. But they estimate that, worldwide, about 1 in 11,000 females and 1 in 7,000 males have fragile X syndrome.
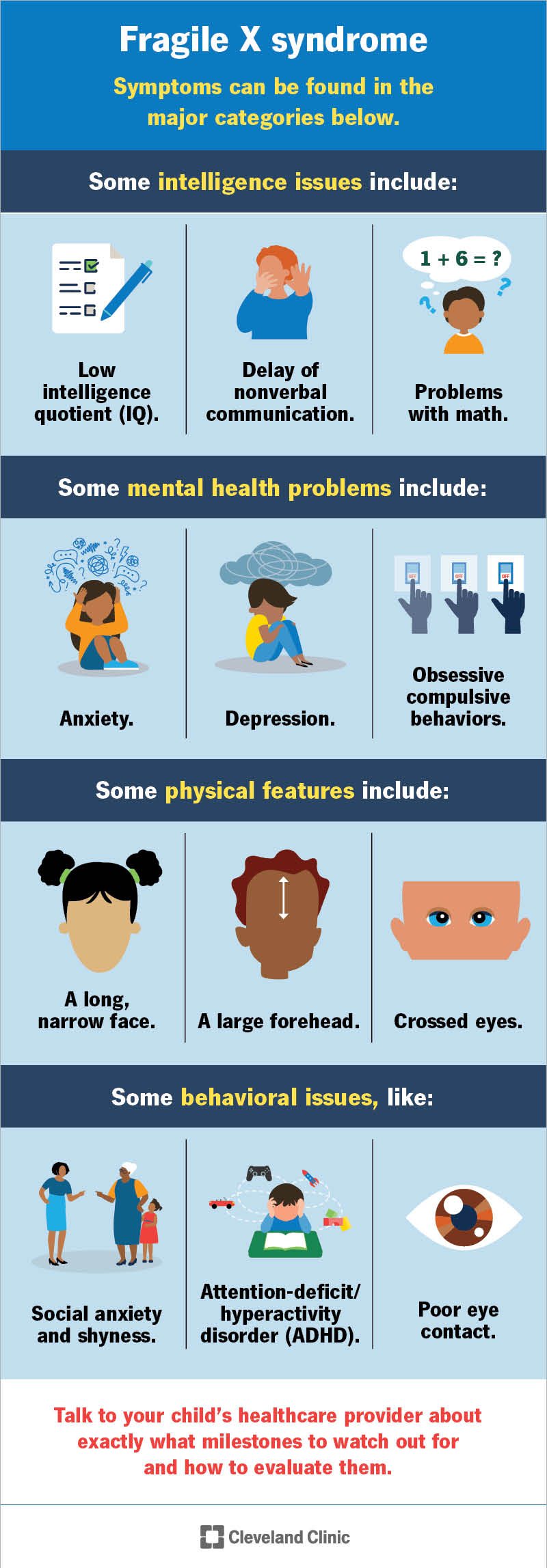
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/fragile-x-syndrome.jpg)
Fragile X syndrome affects your child’s intelligence, mental health, physical features and behavior. Common fragile X syndrome symptoms in each category include:
Talk to your child’s healthcare provider about exactly what milestones to watch out for and how to evaluate them.
Advertisement
Fragile X syndrome may cause a range of behavioral issues, like:
A genetic mutation of the FMR1 gene on the X chromosome causes fragile X syndrome. The FMR1 gene is responsible for providing instructions to your body for making a protein called FMRP. This protein has a vital role in the development of synapses — specialized connections between your nerve cells that are critical for relaying nerve impulses.
A mutation in the FMR1 gene causes a DNA part within it called the CGG triplet repeat to expand. A typical part repeats five to 40 times, but in people with fragile X syndrome, it repeats more than 200 times. This “silences” the FMR1 gene, which disrupts your child’s nervous system and causes the symptoms of fragile X syndrome.
The fragile X syndrome inheritance is in an X-linked dominant pattern. That means the mutated gene that causes it is located on the X chromosome. The inheritance is dominant because only one copy of the mutated gene is necessary to cause the condition.
Fragile X syndrome occurs more frequently in males because they only have one X chromosome. Their symptoms are also more severe. Females have two X chromosomes. The condition may not affect both X chromosomes. Therefore, females can be carriers without having symptoms, but males with fragile X will always have symptoms.
Yes. If your child has fragile X syndrome, you should tell your healthcare provider. As a possible carrier, you’re at a higher risk for:
Sometimes people with fragile X syndrome develop other health conditions. In one study, parents reported that their children also had:
Advertisement
Diagnosing fragile X syndrome requires a DNA sample from your child’s blood or other tissues. Your child’s healthcare provider will send the sample to a laboratory that will determine if your child has the FMR1 gene.
If you’re pregnant and concerned that your child has fragile X syndrome, you can see a genetic counselor where you may undergo the following prenatal tests:
Boys usually receive a diagnosis at 35 to 37 months old. Girls may receive a diagnosis a little later — at about 42 months old. But you may start to notice symptoms in your child as early as 12 months.
Before your child’s healthcare provider or a genetic counselor orders a test for fragile X syndrome, they may ask you the following questions:
While fragile X syndrome is typically diagnosed in children, two other syndromes in the fragile X family may be diagnosed in adults:
Advertisement
If you have symptoms of either of these conditions, talk to a healthcare provider.
Fragile X syndrome doesn’t have a cure, but you can treat the symptoms of the condition. Your child’s healthcare provider may prescribe a variety of fragile X syndrome medications. Examples of medications, categorized by symptom, include:
Seizures or mood instability:
ADHD:
Aggression or obsessive-compulsive disorder:
Sleep issues:
This is just a short list of possible medications your child’s healthcare provider may prescribe. Talk to their provider about possible side effects and complications that may come with each medication.
Advertisement
Your child’s provider will likely also recommend psychotherapy as part of your child’s fragile X syndrome treatment — therapy that helps with coping and behavioral skills.
Some people with fragile X syndrome can live independently. Studies show that about 4 in 10 girls and 1 in 10 boys with fragile X syndrome grow up to have a high level of independence. Girls have the following abilities more than boys:
Fragile X syndrome is generally more severe in boys. About 8 out of 20 girls with fragile X don’t need help with daily activities. The same can be said for only 1 in 20 boys. Most girls get a high school diploma but a majority of boys don’t. Nearly half of women with fragile X have full-time jobs but only 2 in 10 men do.
Your child may need special accommodations at daycare or school. Some parts of the school day and classroom may need to be adjusted to fit their needs. Your child’s teacher might be able to make environmental adjustments and curricular adjustments.
Environmental adjustments:
Curricular adjustments:
Be sure to inform your child’s school that your child has fragile X syndrome. Have a conversation with their teacher about their unique needs. You may also meet with a school psychologist and/or counselor. They work with children 3 years old and older. Other specialists you may want to connect with include:
Talk with your local school and healthcare providers for referrals.
Fragile X syndrome is a lifelong condition. There’s no cure.
None of the symptoms of fragile X syndrome are life-threatening. The fragile X syndrome life expectancy is the same as for the average person.
No, fragile X syndrome is a genetic condition and you can’t prevent it. If you’re pregnant or thinking about becoming pregnant, you may wish to speak with a genetic counselor about your risk of passing on the condition to your child.
Fragile X syndrome affects every child differently. Your child’s healthcare team will be able to give you a better idea of how it’ll affect your child and family. While aspects of the condition can be challenging, there are many positive characteristics. For example, researchers have noted that people with fragile X are:
Educate yourself as much as possible. Look for support groups and community resources that can help you and them. Life skills programs may be appropriate. Some provide guidance about:
It’s important to advocate for your child to make sure they get the care they need and have the best possible quality of life.
Take your child in to see their pediatrician as soon as you notice the symptoms of fragile X syndrome. Don’t wait, as early intervention is important.
The following are some questions you may want to ask your child’s healthcare provider when you discuss their diagnosis:
Fragile X syndrome can be a difficult diagnosis for you and your child. It’s the start of a lot of change and adjustment. Therapy, medications and accommodations at school are now part of your child’s life. While helping your child, be sure not to neglect your own needs. Remember that if your child has fragile X syndrome, that means you’re more vulnerable to depression, migraines and many other health conditions.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have a neurological condition, you want expert advice. At Cleveland Clinic, we’ll work to create a treatment plan that’s right for you.
