Axial spondyloarthritis is a type of inflammatory arthritis that often causes chronic back pain in young adults. There’s no cure, but your provider can help you create a treatment plan to manage it. With the right care, you can get relief from pain and other symptoms and live a full, active life.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
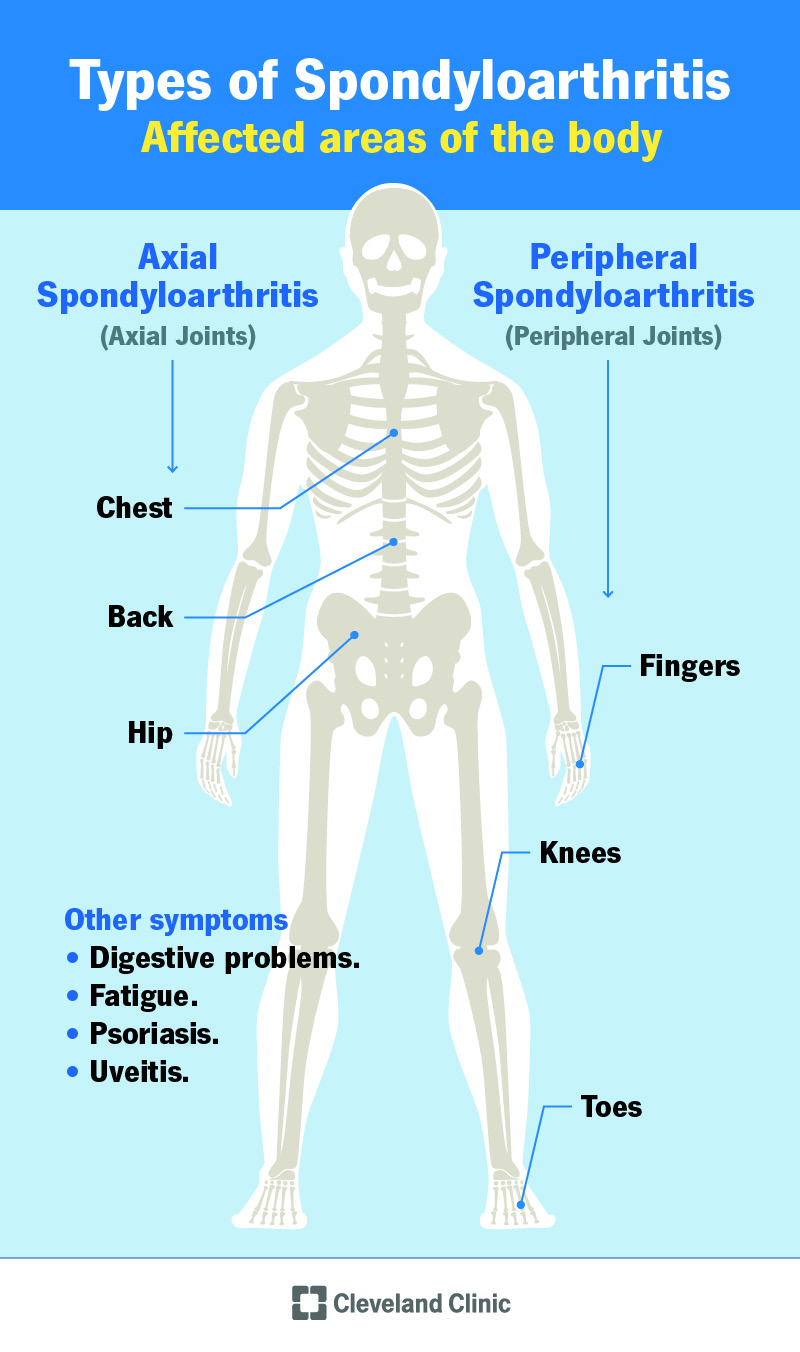
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/24843-axial-spondyloarthritis-infographic)
Axial spondyloarthritis (axSpA) is a type of arthritis that affects the joints in your axial skeleton (chest, spine and pelvis). People with axSpA often have back pain before the age of 45 and may even have stiffness and pain as teens or young adults. This pain can be severe and debilitating.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
AxSpA is a type of spondyloarthritis, which is a group of inflammatory arthritis conditions that cause joint pain and other symptoms. Inflammatory indicates an unregulated or overactive immune system. This causes joint or soft tissue swelling and damage.
Spondyloarthritis is different from other types of arthritis because it can affect other body systems in addition to your joints. If you have axSpA, you might experience eye inflammation, diarrhea or other problems that seem unrelated to joint pain.
Anyone can get axSpA, but it’s rare. This condition affects about 1% of people in the world. It usually occurs in people younger than 40, often starting during your teens or 20s. It occurs equally in males and females.
Over time, untreated axSpA can cause the bones of your spine to fuse together. The name for this fusion is ankylosis, and it can cause osteoporosis in your spine. This can lead to a breakdown of the bones in your spine and raise the risk of a spinal fracture (broken bone in your spine).
AxSpA often runs in families. Most people with axSpA have a gene called HLA-B27. However, some people get axSpA who don’t have this gene or a family history of the condition. And many people with the HLA-B27 gene don’t get axSpA.
Advertisement
The most common symptom of axSpA is back pain that’s:
If you have axSpA, your back pain may also:
The inflammation from axSpA can also affect other systems in your body. For example, people with axSpA may also experience:
When you see your provider about your back pain, they’ll check your vital signs and perform a physical exam. These two things give your provider some general information about your health. Your provider may also perform blood tests to look for the HLA-B27 gene and C-reactive protein, which is a sign of inflammation in your body.
Your provider may also recommend imaging tests to view the bones in your axial skeleton. These tests may include:
Healthcare providers diagnose axSpA if you have back pain and other symptoms of axSpA, even if an imaging test doesn’t show inflammation. If you have symptoms of axSpA but no visible inflammation in the spine, your provider may diagnose non-radiographic axSpA. Non-radiographic means that it can’t be seen on an imaging test like an X-ray or MRI.
Some cases of non-radiographic axSpA can get worse over time, eventually showing up on an X-ray or MRI. But in many cases, non-radiographic axSpA never reaches the point of being visible on imaging tests.
There’s no cure for axSpA. But treatment can help you get relief from symptoms and improve your quality of life. Your treatment may include:
Advertisement
There’s no cure for axSpA. If you have axSpA, your symptoms may come and go, or you might feel them all the time. People with this condition can live long, full lives. Work with your provider so you can manage symptoms and stay as healthy as possible.
There’s no known way to prevent axial spondyloarthritis, and it’s not caused by back injuries.
If you have a parent or sibling with axSpA, you have a higher risk of getting this condition. However, having a family history or the HLA-B27 gene doesn’t mean you’ll get axSpA.
There are a few things you can do to boost your health and manage axSpA symptoms:
Contact your provider if you notice:
Advertisement
Ankylosing spondylitis is a type of axSpA. Ankylosing spondylitis mainly affects the sacroiliac joints, which are the joints that connect the lower part of your spine to your hips. But AxSpA can also affect your chest or other areas of your spine.
Other types of spondyloarthritis include:
Living with axSpA can be challenging, but many people lead long, healthy lives with this condition. You can manage the condition by seeing your provider regularly and taking care of your overall health. Consider joining a support group for people with axSpA and spondyloarthritis. These groups can help you connect with others who understand how you’re feeling and the unique challenges you face.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When you have an inflammatory or autoimmune condition, you need experts by your side. At Cleveland Clinic, we’ll create an individualized treatment plan for you.
