Pustular psoriasis is a type of psoriasis that causes pus-filled blisters on plaques, which are patches of scaly, flaky skin. Pustular psoriasis is common on your hands and feet, but can form anywhere on your body. There isn’t a cure for psoriasis, but treatment is available to help manage symptoms.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
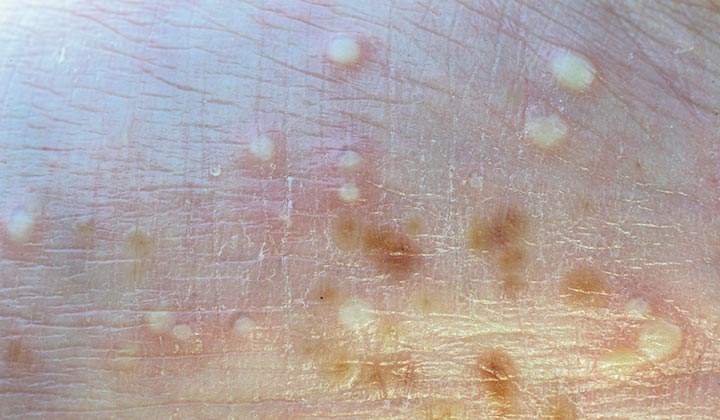
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/24805-pustular-psoriasis)
Pustular psoriasis is a form of psoriasis that looks like scaly, discolored patches of skin with fluid-filled blisters or pustules. Psoriasis can form anywhere on your body. It can be painful and sore if pustules break open. Psoriasis is a chronic condition that can come and go throughout your life.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Pustular psoriasis affects people diagnosed with psoriasis. Psoriasis is a skin condition that affects millions of people in the United States. An estimated 3% of people diagnosed with psoriasis experience pustular psoriasis symptoms at least once during their lifetime. Pustular psoriasis can affect anyone diagnosed with psoriasis at any age, but it’s more common among adults than children.
Pustular psoriasis isn’t rare, but a type of pustular psoriasis called generalized pustular psoriasis is the rarest form of psoriasis. Generalized pustular psoriasis causes symptoms of psoriasis that affect a large area of your body. Additionally, you may have symptoms like a fever and muscle weakness accompanying the quickly spreading psoriasis plaques on your skin.
Pustular psoriasis is a type of psoriasis that causes skin plaques with pustules or blisters anywhere on your body. Palmoplantar pustulosis, which is also known as palmoplantar pustular psoriasis, is pustular psoriasis that affects only your hands and feet.
Pustular dermatosis is a skin condition that causes pus-filled blisters to form under the top layer of your skin (subcorneal layer). These pustules usually form in areas of your skin where there’s friction, like in your groin or underarms. While pustules are the main symptom of both pustular dermatosis and pustular psoriasis, dermatosis doesn’t cause skin plaques of flaky, discolored skin.
Advertisement
There are two types of pustular psoriasis based on how and where they affect the skin on your body:
Signs and symptoms of pustular psoriasis could include:
The pustules on your skin can join together with other fluid-filled bumps and burst open. This can make your skin feel tender and sore. When pustules burst, new pustules can form in the same location.
It’s common for pustular psoriasis to cover a small area of your body, like the palm of your hands, and cause just local symptoms. Although rare, pustules on plaques can cover a large area of your body. This is called generalized pustular psoriasis, and you may experience additional symptoms that could include:
If you experience symptoms of pustular psoriasis and symptoms of generalized pustular psoriasis, contact a healthcare provider immediately.
Symptoms of pustular psoriasis can affect any part of your body where you have skin. Common sites for symptoms include your:
An overactive immune system causes pustular psoriasis. Your immune system keeps your body healthy by defending itself against foreign invaders like bacteria. These invaders can make you sick. If you have psoriasis, your skin immune system becomes overactive and releases inflammatory molecules that cause healthy skin cells to divide and replicate too quickly, which causes dead skin cells to form on the surface of your skin as scales or flakes. This state of immunologic over-activity also causes certain cells from the immune system call neutrophils to collect in the most superficial layers of the skin, which causes pustules.
Advertisement
Irritants or allergens in your environment can trigger symptoms of pustular psoriasis. Common triggers include:
No, pustular psoriasis isn’t contagious. Even though the fluid that can leak out of your pustules looks like an infection, it isn’t. You can’t spread psoriasis to other people through physical contact.
A healthcare provider will diagnose pustular psoriasis after a physical examination. They’ll ask you questions about your symptoms and take a complete medical history. The visual appearance of your symptoms usually leads to an accurate diagnosis, but your symptoms may look similar to other conditions so tests might be necessary. Your provider might offer a culture test, a skin biopsy and/or an allergy test to confirm a diagnosis. If your provider suspects generalized pustular psoriasis, they may also want to collect blood for tests, such as a complete blood count.
You may need to see a dermatologist to diagnose and treat psoriasis.
Treatment for pustular psoriasis focuses on:
Advertisement
A healthcare provider will offer a treatment plan that could include:
It can take a couple of weeks to a few months before your skin completely clears up after a flare-up of symptoms of pustular psoriasis. Treatment usually works in stages to clear the pustules, prevent the build-up of dead skin cells on the surface of your skin that causes scaling and reduce skin discoloration. If you’re concerned about the timeline for your treatment, talk with your healthcare provider so you can feel better sooner.
Psoriasis is a chronic, lifelong condition. You may experience symptoms that come and go throughout your life. There isn’t a cure for pustular psoriasis. Your healthcare provider can help you manage your symptoms and identify triggers.
When you get a flare-up of symptoms, try to keep track of any irritants or allergens that may have triggered it. If you notice patterns when you have symptoms and when you contact certain things or feel stressed, those could be triggers. To avoid recurring flare-ups, avoid those triggers. If you’re having trouble identifying your triggers, talk to a healthcare provider.
Advertisement
You can’t prevent pustular psoriasis, but you can reduce your risk of a flare-up of symptoms by:
Visit your healthcare provider if you:
Visit the emergency room if you have symptoms of generalized pustular psoriasis, which includes pustules on skin plaques in addition to:
Pustular psoriasis can be a frustrating condition to manage, as your symptoms can cause skin irritation that can come and go unexpectedly throughout your life. Some people diagnosed with psoriasis find comfort in speaking with a mental health professional if their symptoms affect their self-confidence or self-esteem. A healthcare provider can help you manage your symptoms. If you experience symptoms of pustular psoriasis and symptoms of generalized pustular psoriasis, like widespread skin plaques, a fever and muscle weakness, visit your healthcare provider immediately.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Coping with psoriasis can be frustrating and distressing. Cleveland Clinic experts offer personalized treatment to help you manage this chronic condition.
