Hemarthrosis is bleeding into the space around one of your joints. It most commonly affects people’s knees, but can happen to any joint that moves (your synovial joints). A healthcare provider will treat the cause of the bleeding. You’ll probably be able to manage symptoms like swelling and pain with at-home treatments.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
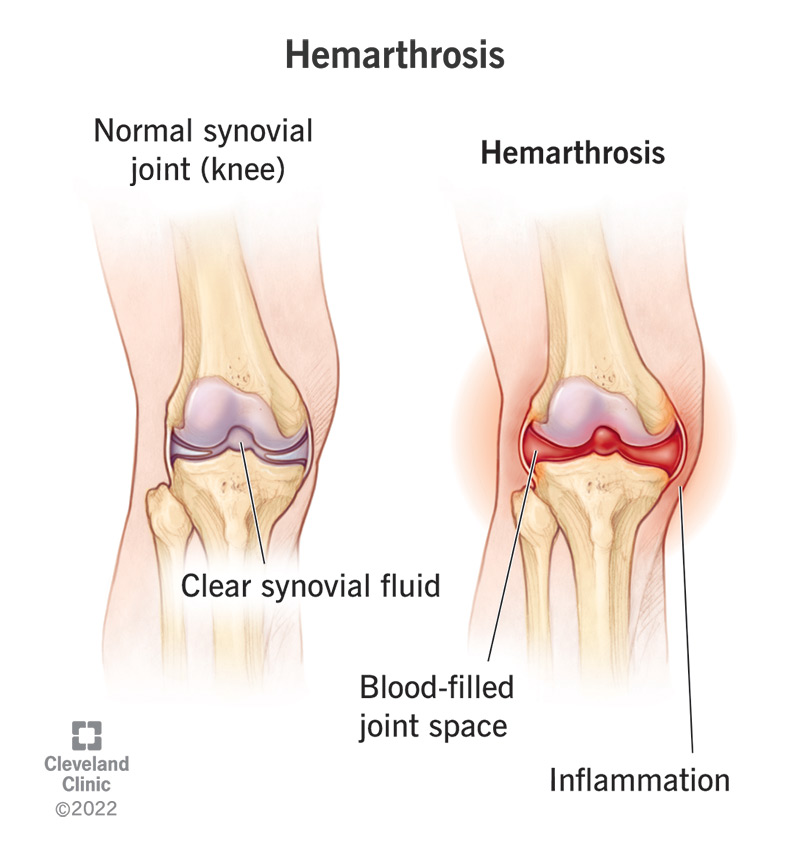
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/24225-hemarthrosis)
Hemarthrosis is the medical term for bleeding that happens inside one of your joints. You might see it referred to as articular bleeding.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Joints are places in your body where bones meet. The joints that help you move are called synovial joints. They’re lined with a synovial membrane — a thin barrier that covers the space where your bones come together.
Your synovial membranes protect the joints they surround. They work with your cartilage, tendons and ligaments to reduce friction between the bones in your joints — especially when you’re moving them.
Hemarthrosis happens when something causes bleeding that leaks into your synovial membrane or the cavity inside one of your joints. It will cause swelling, and might make it hard to use your joint.
Hemarthrosis can develop in any synovial joint in your body, but it usually affects:
Hemarthrosis can be caused by injuries, health conditions, as a side effect of medication and after joint surgeries. A healthcare provider will treat the cause of the bleeding and any symptoms you’re experiencing. Most people recover in a few weeks, depending on what caused the hemarthrosis.
You might have acute hemarthrosis — bleeding into a joint that’s temporary and caused by an injury or short-term illness. If you have a bleeding disorder that causes hemarthrosis to come back (recur) a healthcare provider may diagnose you with chronic hemarthrosis.
Advertisement
Visit a healthcare provider if you’re experiencing swelling around one of your joints — especially if it hurts or makes it hard to move.
Hemarthrosis can affect anyone. If you experience a trauma that affects one of your synovial joints, you might develop hemarthrosis.
People with certain health conditions are more likely to experience hemarthrosis, including:
It’s hard to estimate how common hemarthrosis is because it’s caused by many issues and conditions.
Studies have found that around half of all people with hemophilia will experience hemarthrosis at some point.
Half of all cases of hemarthrosis in knees are caused by ACL tears and other damage to knee ligaments.
The most common symptoms of hemarthrosis include:
The most common causes of hemarthrosis include:
You might also experience hemarthrosis after you have surgery on one of your joints, including:
A healthcare provider will diagnose hemarthrosis with a physical exam and imaging tests. They’ll look at your affected joint and ask you about symptoms you’re experiencing.
They might check your range of motion (how far you can move a joint) and compare it to another healthy joint. For example, they’ll compare how far you can move your affected knee to your healthy knee. They might take a blood sample to check for an infection.
You might need one of a few imaging tests, including:
Your provider may perform a joint aspiration (arthrocentesis). They’ll remove some of the excess fluid from around your joint and send it to a lab for testing.
Diagnosing hemarthrosis is usually part of a differential diagnosis — a list of conditions that share the same symptoms to help make a final diagnosis. Lots of issues and conditions cause swelling, so your provider will rule out other causes of your symptoms before diagnosing you with hemarthrosis.
Advertisement
Your provider will treat the cause of the bleeding as well as the symptoms you’re experiencing. Usually, stopping the bleeding inside your joint will prevent your hemarthrosis symptoms from getting any worse. Which treatments you’ll need depends on what’s causing the bleeding. Your provider or surgeon will tell you what to expect. You may need a blood transfusion.
Usually, you can treat symptoms of hemarthrosis at home while you’re waiting for your joint to heal. You can use the RICE method. RICE stands for Rest, Ice, Compression and Elevation.
Talk to your provider before taking any over-the-counter pain relievers (analgesics). Many common medications (including NSAIDs like aspirin, ibuprofen and naproxen) can thin your blood and make the hemarthrosis worse.
Advertisement
How long it takes to recover from hemarthrosis depends on what caused the bleeding into your joint. Some people recover in a few days if the bleeding stops quickly. Other cases of hemarthrosis take a few weeks to heal.
If the hemarthrosis was caused by a trauma like a bone fracture, you might take longer to recover. Talk to your provider or surgeon about what to expect. Ask them when you can start using your joint, and when it’s safe to resume physical activities.
You can’t prevent hemarthrosis because you can’t prevent the health conditions that cause it — and there’s no way to know when you’ll experience a trauma.
Visit a healthcare provider as soon as you notice any new swelling in or around one of your joints, especially if you have a bleeding disorder.
Go the emergency room if you’ve experienced a trauma or suddenly can’t move one of your joints.
Both hemarthrosis and joint effusion cause swelling around one of your joints.
Joint effusion happens when extra fluids flood the tissues around your joint. It’s a general term for any swelling in the area around of your joints. It can be caused by everything from injuries, overuse or infections. The fluid buildup might contain some blood, but it’s not only caused by bleeding.
Advertisement
Hemarthrosis occurs when something causes your body to bleed into your joint and the space around it. The swelling is caused by bleeding into your joint that leads to a buildup of blood in and around it.
Visit a provider if you notice new swelling around one of your joints.
Hemarthrosis happens when bleeding inside your body makes blood pool around one of your joints. It’s important to get the bleeding stopped and its cause treated. Visit a healthcare provider as soon as you notice any swelling or bruising around one of your joints — especially if you’re in pain or it’s hard to move.
Even though you can treat some hemarthrosis symptoms at home, talk to a provider before taking any over-the-counter medications to treat pain or swelling. Many of the most common pain relievers can thin your blood and make the bleeding that caused hemarthrosis worse.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
From sudden injuries to chronic conditions, Cleveland Clinic’s orthopaedic providers can guide you through testing, treatment and beyond.
