Tenosynovitis is inflammation of the connective tissue that protects your tendons. When this tissue (also called a tendon sheath) is overused, it can become inflamed, leading to pain and stiffness. If you have symptoms of tenosynovitis, be sure to rest the affected body part and see your provider. Untreated tenosynovitis can lead to complications.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
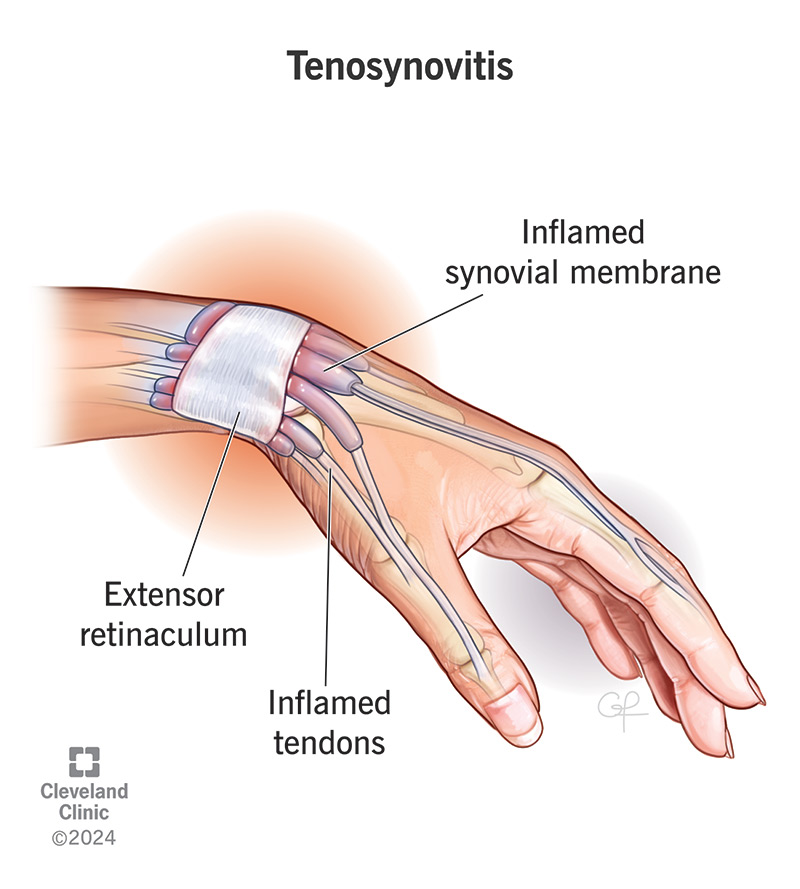
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/tenosynovitis)
Tenosynovitis (pronounced “ten-oh-sin-oh-vyt-us”) is inflammation of the thin layer of tissue (your synovial membrane) that surrounds your tendons. The condition can be painful and make it hard for you to move your joints like you usually can.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your tendons are cords that connect your muscles to your bones. They let your bones move as you tighten and relax your muscles. Your synovial membrane is full of fluid. It protects your tendons and helps them move smoothly.
When something irritates, damages or infects your synovial membrane, inflammation can occur. In addition to symptoms from the tenosynovitis itself, this inflammation can lead to other serious issues if you don’t seek treatment. You’ll usually need to rest your affected tendon while it heals.
Healthcare providers classify tenosynovitis in a few ways:
The most common tenosynovitis symptoms include:
Advertisement
Tenosynovitis is usually painful. It can affect tendons connected to any muscle that helps one of your limbs push, pull, bend or straighten (your flexor and extensor muscles). You might also have trouble moving the affected part of your body like you usually can. The most common places tenosynovitis affects include your:
Tenosynovitis causes include:
Tenosynovitis can affect anyone. You’re more likely to develop tenosynovitis if you have:
Tenosynovitis can be a serious condition because it can lead to complications, including:
To diagnose tenosynovitis, your healthcare provider starts with a history and physical exam. They’ll check your symptoms and your range of motion (how far you can move a part of your body). They might also order blood tests or other labs to check for infections and inflammation.
After a physical exam, you might need at least one imaging test to confirm or show the extent of your disease. Imaging tests can also ensure there’s not another problem causing pain and stiffness, like a fracture or dislocation. These tests can include:
How tenosynovitis is treated depends on what’s causing it. Tenosynovitis treatment can include:
Advertisement
Your provider will tell you which specific treatments you’ll need based on how severe your symptoms are.
Which medications you’ll need depends on the cause of the tenosynovitis. Some medications your provider might prescribe include:
The outlook for tenosynovitis is generally positive, depending on the cause. Almost everyone who develops it makes a full recovery and resumes their normal activities. You might need to take a break from the activity that caused you to overuse your tendon, but — once you’ve healed — you should have no long-term effects. Most people recover within a few weeks, even if they need surgery.
Advertisement
If an infection caused the tenosynovitis, your outcome depends on several factors. People who are older or have a history of diabetes, peripheral vascular disease and/or kidney disease have a higher risk of complications and a longer recovery time. A delay in diagnosis or treatment of infectious tenosynovitis may also cause permanent damage.
The best way to reduce your risk of tenosynovitis is to avoid overusing your tendons. Give your body time to recover after workouts, sports, jobs or other activities that require you to perform the same movements repeatedly.
You can prevent strain on your body (including your tendons) by wearing proper safety equipment. It’s also important to work out safely and avoid too much stress on your tendons.
Make sure you’re following all the instructions from your provider or surgeon. Because the most common treatments for tenosynovitis take time to work, it’s important to be patient and let your body heal.
Talk to your healthcare provider if your symptoms get worse or aren’t getting better after a few weeks. Go to the emergency room if you notice any of the following:
Questions you may want to ask your provider include:
Advertisement
Tenosynovitis is painful and can be dangerous if you don’t seek treatment right away. But most people make a full recovery, and you’ll likely only need conservative treatments like rest to give your body time to heal. Don’t “play through the pain” or push your body beyond its limits. If you notice symptoms, talk to your healthcare provider right away.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic experts are here to treat your tendinopathy (tendon pain) and get you back to doing the things you love.
