Left ventricular non-compaction cardiomyopathy is a rare heart condition. It’s typically a congenital issue, meaning you’re born with it. In LVNC cardiomyopathy, your lower left heart chamber doesn’t develop properly. As a result, your heart may not pump blood through your body as efficiently as it should.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
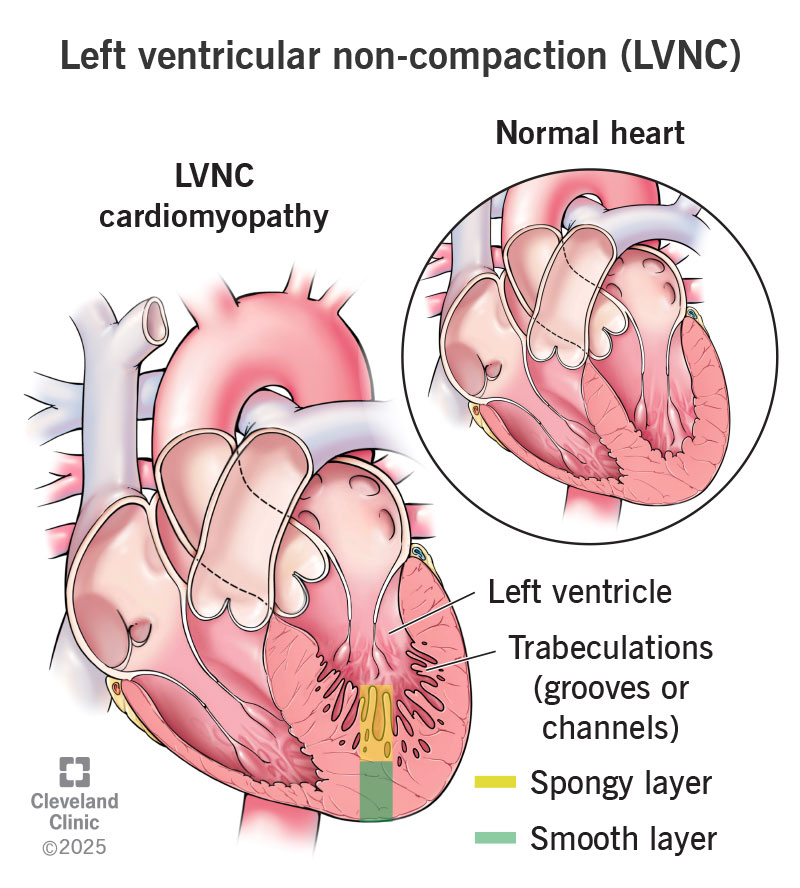
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/23248-left-ventricular-non-compaction-lvnc.jpg)
Left ventricular non-compaction (LVNC) cardiomyopathy is a condition in which your lower left heart chamber (left ventricle) doesn’t develop properly. Instead of being firm and smooth, your left ventricle is spongy and thick. This is because your spongy layer of heart muscle is bigger than it should be — and bigger than your smooth (compacted) layer. The abnormal layer also has grooves or channels (trabeculations). These are visible in diagnostic images of your heart.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
LVNC cardiomyopathy is typically a congenital heart condition. This means you’re born with it. Without treatment, LVNC can lead to serious heart problems.
Usually, your left ventricle pumps oxygen-rich blood from your lungs to the rest of your body. With LVNC, your left ventricle can’t contract and relax as it should. As a result, your heart can’t efficiently pump blood throughout your body. This condition may also result in abnormal heart rhythms (arrhythmias) or sudden cardiac death.
Left ventricular non-compaction is rare. Experts estimate that only up to 12 in 1 million people get an LVNC diagnosis each year. The actual number of people with the condition may be higher. People who don’t have symptoms may not have a diagnosis.
LVNC symptoms can range from mild to severe. Many people with left ventricular non-compaction have no symptoms. Others may have:
Usually, you develop LVNC cardiomyopathy because of a gene change (variation) you have before you’re born. This gene change may occur randomly, or you may inherit it from one or both biological parents.
Advertisement
LVNC can also have an association with other forms of congenital heart disease and cardiomyopathy, as well as with genetic syndromes like Fabry disease or neuromuscular disorders. Variants that cause left ventricular non-compaction may happen in genes involved in the production of cardiac proteins. Genetic testing can confirm that you have these variants.
But LV non-compaction isn’t always genetic. Some females develop LVNC cardiomyopathy for no known reason during their first pregnancy. Experts think this may occur because pregnancy can put extra stress on your heart muscle. In some, symptoms go away after pregnancy. Others deal with LVNC cardiomyopathy long-term.
Some athletes and people with sickle cell anemia or kidney issues may also have extra non-compacted muscle.
Often, experts don’t know the cause of left ventricular non-compaction cardiomyopathy. Healthcare providers describe LVNC as isolated when you don’t have symptoms or a known genetic cause. Other LVNC types have links to certain syndromes, forms of heart muscle disease and heart issues present at birth.
LVNC cardiomyopathy happens more often in males. This condition may also have a link to heart problems present at birth, like certain valve issues or abnormal holes inside your heart. Certain conditions can also put you at a higher risk of LVNC, like:
Physical activity may set off abnormal heart rhythms. Some people develop severe heart problems, including sudden cardiac death. This is when your heart suddenly stops beating.
About 2 in 3 people with LVNC cardiomyopathy will develop heart failure. Blood clots are possible, as well. They can cause a stroke, TIA, heart attack or other issues.
You can get an LVNC diagnosis as an infant, child or adult. Your healthcare provider will likely start with a physical exam and medical history. Then, they’ll use several tests to diagnose LV non-compaction, including:
LVNC treatment varies depending on the symptoms you have. You may not need treatment if you don’t have symptoms.
Your provider will likely tell you to limit your physical activity. Exerting yourself can lead to dangerous heart rhythms.
Advertisement
In some cases, you can reverse LVNC cardiomyopathy. People who get this condition because of pregnancy, sickle cell anemia or athletics can often reverse it. If you can’t reverse LVNC, medicines or a procedure can improve your quality of life, help you manage symptoms and lower your risk of complications.
Your healthcare provider may prescribe medicines like:
Your provider may suggest a procedure, like a (an):
Recovery time varies for these procedures. You may spend a few days in the hospital after getting a device, but you’ll be there more than a week after a heart transplant.
Contact your provider if medicines or other treatments aren’t helping you. You’ll likely also need regular checkups. These may include an annual EKG. If you don’t have symptoms, you may need to get an echocardiogram every few years to monitor the condition.
If you have left ventricular non-compaction, or you think you could, you may want to ask your healthcare provider:
Advertisement
The outlook for LVNC cardiomyopathy varies. The prognosis is worse for people with abnormal heart rhythms, blood clots that cause issues and a left ventricle that isn’t working well. Some people with LVNC have a typical life expectancy.
Left ventricular non-compaction cardiomyopathy can be fatal. But it often isn’t. Most people who have it don’t die from the disease. It’s important to have regular visits with a heart expert. They can help you manage your heart health to lower your risk of having more heart problems.
Symptoms like having trouble catching your breath make everyday life difficult. If you have LVNC cardiomyopathy, it’s important to have regular visits with your healthcare provider. They can give you treatments to reduce your risk of future issues and improve your quality of life.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Whether you were diagnosed as a child or later in life, Cleveland Clinic is here to treat your adult congenital heart disease.
