Coronary artery calcification is a buildup of calcium that can predict your cardiovascular risk. Symptoms like chest pain usually don’t happen until you’ve had it for a while. Your healthcare provider has several options to remove the calcifications narrowing your coronary artery. Success rates are high, but there are risks with each treatment.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
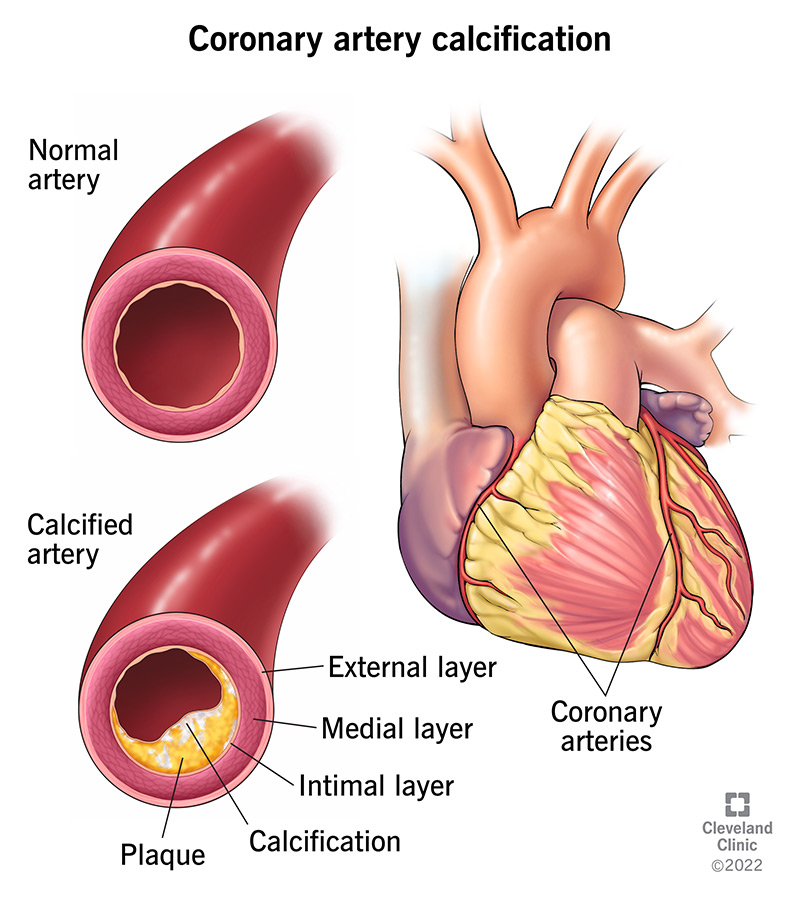
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22953-coronary-artery-calcification)
Coronary artery calcification is a collection of calcium in your heart’s two main arteries, also called your coronary arteries. This happens after you've had plaque (fat and cholesterol) forming in your arteries (atherosclerosis) for about five years.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Coronary artery calcification is an indicator of coronary artery disease and can give your healthcare provider information to help them assess your cardiovascular risk.
When plaque accumulates in your arteries, it makes it harder for blood to get through. Good blood flow is crucial in your coronary arteries because they supply oxygen-rich blood to your heart muscle. If blood can’t get through your coronary arteries, it can lead to chest pain and/or a heart attack.
The amount of calcification you have is an indicator of how bad your atherosclerosis may be. Atherosclerosis is the result of plaque collecting in your arteries, making them narrow. This makes it difficult for blood to get through your arteries.
People who have coronary heart disease usually have coronary artery calcification.
In people older than 70, more than 90% of men and 67% of women have coronary artery calcification. Before menopause, estrogen protects women from developing atherosclerosis. This is why women tend to develop atherosclerosis 10 to 15 years later than men.
People who are white are more likely than other races to have coronary artery calcification.
Advertisement
You’re more likely to get coronary artery calcification if you have:
Men also have a higher risk for coronary artery calcification.
Coronary artery calcification makes your arteries stiff and less able to expand and contract. This puts you at a higher risk for cardiovascular issues.
Coronary artery calcification causes less blood to get to your heart muscle.
Calcification makes it difficult for your healthcare provider to do percutaneous coronary intervention (PCI) or angioplasty. It makes it harder to expand a stent to keep your artery open.
People with coronary artery calcification often don’t have any symptoms. Over time, people may get symptoms, such as:
After age 40, calcium from your bloodstream can settle in parts of your body. Damaged, inflamed or repaired arteries are more likely to attract calcium deposits. This process can start in your 20s, but your healthcare provider may not see it until there’s an amount large enough to show up on imaging. And most people in their 20s and 30s wouldn’t have a reason to get imaging.
Calcium deposits start small (.5μm or micron/micrometer) and grow to be larger than 3mm with plaque continuing to accumulate at the same time.
Researchers believe that microcalcification in the intimal layer starts when smooth muscle cells die.
A type of imaging called computed tomography or multidetector computed tomography (MDCT) can find coronary atherosclerosis before it becomes advanced.
A cardiac CT (computed tomography) scan can show calcified plaque deposits in your coronary arteries. This is called a coronary artery calcium (CAC) test, which looks at:
Your healthcare provider will multiply your calcification area by its density to get an Agatston score. You get a score of 0 to 400 or more, with higher scores indicating a larger risk of a heart attack or stroke in 10 years.
Providers have found the CAC test accurately predicts future cardiovascular risk.
You may have to pay for this test out of your own pocket.
More invasive methods to check your coronary artery calcification include:
Advertisement
Although healthcare providers don’t have a standard treatment for coronary artery calcification, some are using intravascular lithotripsy to treat severe cases. This newer procedure uses a catheter (tube) with a device at the end that sends pressure waves out to make the calcification come apart. After the procedure, your provider can put in a stent (small metal tube) to keep your artery open.
Other treatments to improve artery blood flow:
Advertisement
Rotational atherectomy complications may include:
Coronary angioplasty complications may include:
If you have coronary artery calcification, you’re at a high risk of developing coronary artery disease and major adverse cardiovascular events (MACE).
Intravascular lithotripsy was successful in more than 92% of cases, and rotational atherectomy has had a 90% success rate.
Coronary artery calcification increases the chances that a balloon angioplasty will fail. It also makes it more difficult to put a stent in a position where it would work best.
You can reduce your risk of coronary artery calcification by treating the problems that put you at risk for it. These include:
If you have coronary artery calcification, you should follow the recommendations for a heart-healthy lifestyle, including:
If you have high blood pressure and/or high cholesterol, you should see your healthcare provider regularly to make sure you’re controlling those issues. See your healthcare provider if you need a plan for how to improve your cardiovascular health.
Advertisement
Call 911 if you’re having chest pain, nausea and vomiting, shortness of breath or other signs of a heart attack.
Knowing if you have coronary artery calcification can help your healthcare provider make a plan for how to help you. You may need a procedure to clear calcium deposits out of your coronary arteries or you just may need to pick up heart-healthy habits. Even if you don’t have cardiovascular issues, you can eat less fat, exercise more and avoid tobacco products to help keep yourself healthy.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When you need treatment for coronary artery disease, you want expert care. At Cleveland Clinic, we’ll create a treatment plan that’s personalized to you.
