Tendinopathy causes chronic pain and declining functionality in a tendon. It gets worse the more you try to use it. It needs time and rest to heal. If you have persistent or worsening symptoms in a tendon, a healthcare provider can tell you what type of tendinopathy you have and what type of treatment you’ll need to recover.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
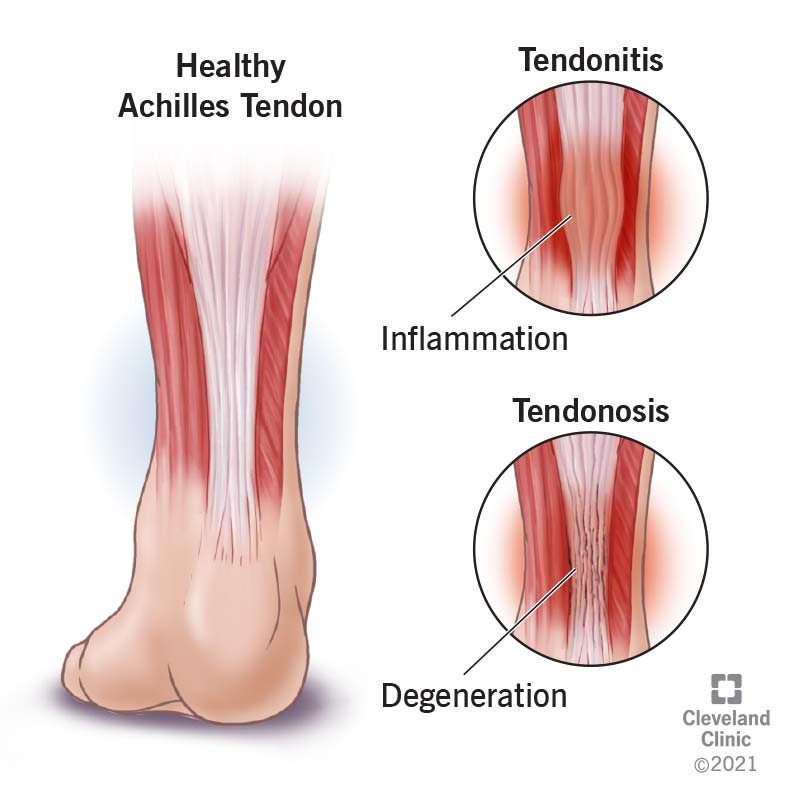
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/22289-tendinopathy)
Tendinopathy is any condition that affects a tendon, making it painful to use and reducing its functionality. Tendons are rope-like connective tissues that attach muscles to bones. Most people injure their tendons by overusing them — although other factors can contribute to weakening of your tendons. Tendinopathy can begin when a tendon injury can’t heal. Eventually, destructive changes begin to occur.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Tendinitis and tendinosis are two different types of tendinopathy. While they often begin in a similar way, they affect your tendons by different processes. They also have different treatment protocols.
Tendinitis is inflammation in your tendon. It’s usually an acute response to an injury. But it can become chronic if the injury doesn’t heal. If inflammation lasts too long, it can be destructive.
Chronic tendinitis can lead to:
Tendinosis is a breakdown of the collagen in your tendon, which makes it lose its strength and elasticity. It happens separately from inflammation. The process is progressive and lasting.
Untreated tendinosis can lead to:
When symptoms first develop, most people don’t know what type of tendinopathy they have — only where it hurts. You might simply say that you have “shoulder tendinopathy” or “ankle tendinopathy.”
Tendinopathy is most common in your:
Advertisement
As many tendon injuries begin as sports injuries, it’s common to refer to a sore tendon by the name of the sport that can cause it. However, you may still develop this tendon injury without playing a sport.
Examples include:
Tendinopathy is characterized by:
Depending on the type, it may also cause:
It’s not always clear how tendinopathy develops, but it often starts with overusing your tendon. How much force your tendon can tolerate may differ from the next person. Athletes can strain their tendons by overtraining. People who aren’t regularly active can strain a tendon by suddenly increasing their activity. Any task repeated too often without enough rest in between can cause a repetitive strain injury.
Examples of repetitive tasks include:
Factors that may contribute to straining your tendon include:
In addition, some medications can cause tendon damage as a side effect, including:
When you strain your tendon, small tears in the fibers can form. Tendons are strong, but when they tear, they’re slow to heal. Acute inflammation (tendinitis) is your body’s way of starting the healing process. But if your tendon doesn’t get the rest it needs to heal, chronic tendinopathy can set in. Tendinitis might continue long-term, or tendinosis might begin the process of remodeling your tendon.
If you have tendon pain with activity that lasts for several months, you have tendinopathy. But it’s important to find out what kind you have. A healthcare provider can diagnose your tendinopathy with a physical exam and imaging studies. They’ll ask about your symptoms, activities and any recent changes. They’ll examine your tendon and may follow up with imaging to look for signs of tissue changes.
Treatment for different types of tendinopathy can vary, which is why it’s important to get an accurate diagnosis. Treatment can also vary by how long you’ve had tendinopathy and how far it’s progressed. Healthcare providers usually begin with conservative therapies, like rest, ice, anti-inflammatory medications and physical therapy. If these don’t help enough, they may suggest other interventions, such as:
Advertisement
Recovery from acute tendinitis only takes a few days to weeks, but recovery from chronic tendinitis can take up to six weeks. Tendinosis recovery can take much longer — between two and six months. Recovery depends on being able to relieve the strain on your tendon long enough for healing to take place. Follow your healthcare provider’s advice on rest and exercise to ensure a smooth recovery.
You can’t prevent tendinopathy altogether. For example, accidents can happen to you while you’re playing or working. But you can take some steps to reduce your risk of tendinopathy.
To reduce your risk of tendinopathy, work with a trainer or coach. A change in how you play or a different way to stretch could help the same tendons.
If you have tendinopathy:
Advertisement
Tendinopathy is common, and contrary to popular belief, it doesn’t just happen to athletes. Many factors can affect your tendon health, many of which you may be unaware of. Anyone can accidentally injure a tendon. It’s what you do next that matters. Once you’ve recognized the injury, it’s time to shift gears. Tendons are tough and hardworking, but when they’re injured, it’s our turn to take care of them.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic experts are here to treat your tendinopathy (tendon pain) and get you back to doing the things you love.
