Posterior tibial tendon dysfunction (PTTD) is a painful condition that affects the foot and ankle. It can affect your ability to walk or perform certain lower-body movements. PTTD can be treated through nonsurgical or surgical methods.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
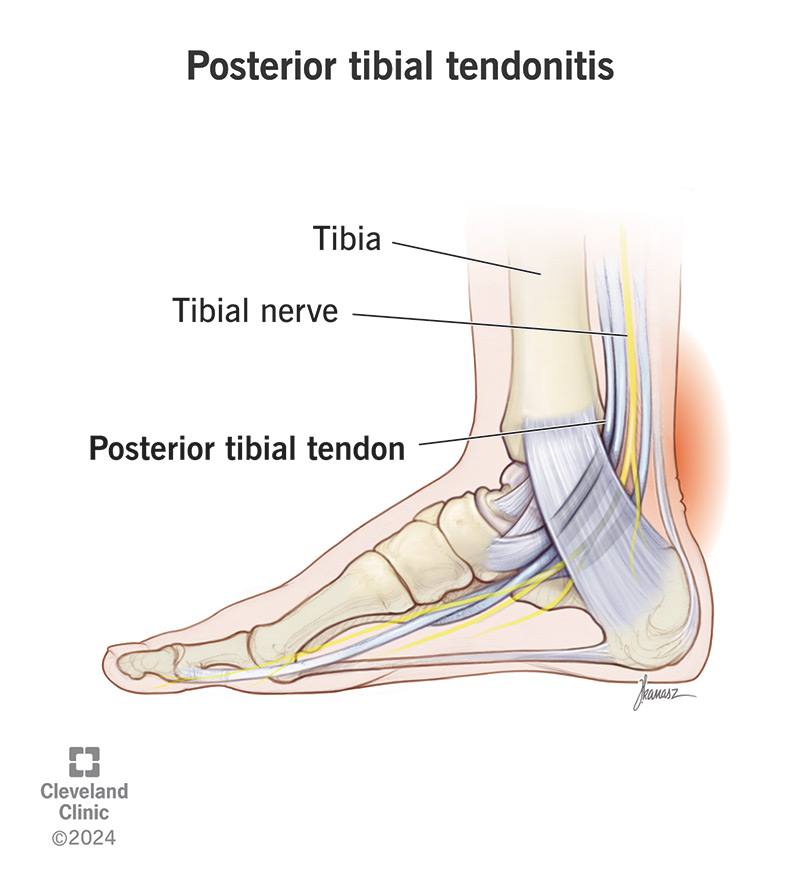
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/posterior-tibial-tendonitis)
Posterior tibial tendonitis is inflammation in your posterior tibial tendon, the tendon that supports the arch of your foot and helps your foot flex. It’s also called your posterior tibialis tendon.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Tendons are tough, rope-like connective tissues that attach muscles to bones. Your posterior tibial tendon connects one of your lower leg muscles to the bones on the inner side of your foot and ankle.
When this tendon is inflamed, you’ll feel pain and tenderness along the arch or the inside of your foot and ankle. Inflammation in a tendon (tendonitis) can be temporary (acute) or long-lasting (chronic).
Posterior tibial tendonitis that lasts too long can start to break down and weaken the tendon. This is called tendinosis. Posterior tibial tendinosis can lead to posterior tibial tendon dysfunction (PTTD).
Posterior tibial tendon dysfunction happens when chronic tendinosis in your posterior tibial tendon causes the tendon to break down. As it weakens, it can no longer support the arch of your foot.
This can make your foot flatten and your ankle turn inward. You might notice your arch and ankle feel weak, especially if you try to lift your heel. If the condition continues, it can progressively worsen.
Healthcare providers also call this posterior tibial tendon insufficiency (PTTI). It’s the leading cause of progressive collapsing foot deformity (PCFD), formerly known as adult-acquired flatfoot or “fallen arch.”
Advertisement
When the arch of your foot collapses, it changes the way your foot bears your weight when you walk. This can injure other parts of your foot over time, including the ligaments and, eventually, the cartilage.
Healthcare providers will stage your condition as follows:
Posterior tibial tendonitis causes pain along the path of the tendon, which travels from the back of your ankle across the inside of your foot, passing behind the bony bump just before your arch.
You might feel it especially during or after activities like walking, running and stair climbing. In the beginning, you might only feel it occasionally, but as it gets worse, you might feel it more often.
Other symptoms of posterior tibial tendonitis may include:
As tendonitis progresses to tendinosis, you may notice that using your foot becomes increasingly difficult, and the pain seems to spread. Eventually, you may notice physical changes in your foot, like:
These are signs of posterior tibial tendon dysfunction.
Injuries are usually the cause of tendinitis. When it comes to foot tendonitis in particular, repetitive strain injuries are the most common cause. We all use our feet often, whether we’re athletes or not.
Overuse of any tendon can strain it, causing tiny tears in the fibers that take a long time to heal. Inflammation is a sign that it’s trying to recover. But if you don’t give it a chance to heal, it won’t.
Advertisement
Sometimes, an acute injury tears your posterior tibial tendon, like a sports injury or a fall that twists your ankle. If the tear doesn’t heal all the way, the acute inflammation can become chronic (ongoing).
Sometimes, an abnormal walking gait contributes to repetitive strain on your tendon. For example, if your foot turns inward or outward, or you have flat feet or high arches, normal walking can strain it.
Risk factors that may contribute to strain and inflammation in your tendon include:
Tendonitis and tendinosis can become a vicious cycle. Chronic inflammation makes the tendon weaker and easier to injure. Repeated injury weakens it further and makes the inflammation continue.
As the tendon becomes less sufficient, other structures in your foot and ankle have to take up the slack. The extra stress on these structures makes them also begin to fail, shifting weight back to your tendon.
Advertisement
Acute posterior tibial tendonitis can heal with time and rest. But if tendonitis becomes chronic, it can start a cycle of tissue degeneration that can eventually lead to posterior tibial tendon dysfunction.
Posterior tibial tendon insufficiency leads to the gradual collapse of your foot arch (progressive collapsing foot deformity, or adult-acquired flatfoot). This can cause additional complications.
Walking on a flat foot will cause your foot ligaments, and eventually, bones, to shift out of place, leading to further foot deformities. These deformities stress your joints, leading to foot and ankle arthritis.
Another possible complication is a complete rupture of the tendon. Progressive weakening of the tendon makes it easier for an acute injury to tear it completely. A complete tear will need surgery to fix.
Conditions affecting your posterior tibial tendon (tendinopathy) will usually be evident on a physical exam. A healthcare provider will examine your foot and ankle as you stand and move it different ways.
They might feel around the tendon for swelling and apply pressure to see if it’s tender. They might follow up with imaging tests, like an X-ray or ultrasound, to see your condition in more detail.
Advertisement
In the early stages, you can treat posterior tibial tendonitis conservatively with rest, ice, and over-the-counter medications. In more severe cases, you might need to wear a cast or boot for a few weeks.
Conservative treatments for PTTD include physical therapy and wearing special orthotics to take stress off your tendon when you walk. In more severe cases, you might need surgery to fix your foot.
For all stages, healthcare providers begin with conservative (nonsurgical) treatments. If these treatments don’t improve your symptoms after several months, they’ll consider surgical treatments.
An acute case of tendonitis can heal in a few weeks. But if you have tendinosis and tendon dysfunction, it’ll take longer. With conservative treatments, it may take three or four months to fully recover.
If conservative therapy isn’t working after several months, your provider will offer surgical treatments. Following surgery, you may need another two to four months to recover and rehabilitate your tendon.
The outlook for PTTD depends on the stage of your condition and the type of treatment you need. In the earlier stages of the condition, most people can fully recover with conservative therapy.
If you need surgery to reconstruct parts of your foot, the outcome is less predictable. Surgery can be complex and may involve multiple procedures. After surgery, you may still have some lingering effects.
You can help prevent tendonitis and tendinosis by taking care not to overstress your tendon. If you know that you ask a lot of your feet, make sure to wear supportive shoes and rest them well afterward.
If you start to feel sore in your tendon, pay attention and let it rest and recover. See a healthcare provider if your symptoms continue. They’ll let you know if you have tendonitis and what to do.
If you receive a diagnosis of tendonitis or tendinosis, it’s very important to follow your provider’s advice. Not giving your tendon a chance to recover properly will only prolong your symptoms and recovery.
Posterior tibial tendon dysfunction happens when tendonitis and tendinosis last for a long time. Some people don’t notice symptoms in the early stages. But when you do notice, it’s important to treat it.
As much as we all rely on our feet, it’s easy to take them for granted. If they hurt, we might feel that’s the cost of living. But you might be surprised to learn how important a small tendon in your foot can be.
Tendons are tough, but when they’re injured, they heal slowly. If they don’t heal, chronic inflammation can wear them down. And if your posterior tibialis tendon fails, the structure of your foot falls apart.
The moral of the story is, take your pain seriously. The sooner you can get proper care for posterior tibial tendonitis and posterior tibial tendon dysfunction, the smoother your recovery is likely to be.
Recovery can take some time, especially if you need surgery. It’s frustrating to stop everything for a tiny tendon. If it helps, just think of it as payback for all the work this tiny tendon does for you every day.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic offers treatment for ankle arthritis, bursitis, sprained ankles and other causes of ankle pain — often without surgery.
